Mini gastric bypass surgery has emerged as a significant advancement in bariatric procedures, offering patients substantial weight loss results with shorter operating times compared to traditional techniques. Despite its growing popularity and efficacy, this procedure carries a range of potential complications that patients and healthcare providers must carefully consider. Clinical studies indicate that approximately 5-15% of patients experience some form of complication following mini bypass surgery, ranging from mild discomfort to severe conditions requiring immediate medical intervention. These complications can manifest immediately post-operation or develop months to years after the procedure, necessitating ongoing monitoring and proactive management strategies.
Table of Contents
The spectrum of mini bypass complications includes both surgical and metabolic issues that vary in severity and prevalence. Surgical complications such as anastomotic leaks, intestinal obstruction, and internal hernias occur in approximately 1-3% of cases, while metabolic complications like nutritional deficiencies, dumping syndrome, and bile reflux affect a larger percentage of patients. Research published in the Journal of Bariatric Surgery demonstrates that hospitals performing higher volumes of these procedures typically report lower complication rates, suggesting that surgeon experience and institutional protocols significantly influence patient outcomes. The risk profile also varies based on patient characteristics including age, pre-existing conditions, and baseline BMI, creating a complex clinical landscape that requires personalized pre-operative assessment and tailored post-operative care.
Mini Gastric Bypass Outcomes and Success Rates
The mini gastric bypass (MGB) has established itself as a highly effective bariatric procedure with impressive success rates in both weight loss and metabolic improvement. Research indicates this procedure delivers consistent long-term results that significantly transform patients’ lives.
- Average Weight Loss: Patients typically lose 60-80% of excess weight within the first year
- Metabolic Improvements: 85% of patients experience type 2 diabetes remission
- Procedure Duration: Usually completed in 45-60 minutes (shorter than traditional bypass)
- Hospital Stay: Typically 1-2 days compared to 2-4 days for standard bypass
- Long-term Success: 70-75% of excess weight loss maintained at 5-year follow-up
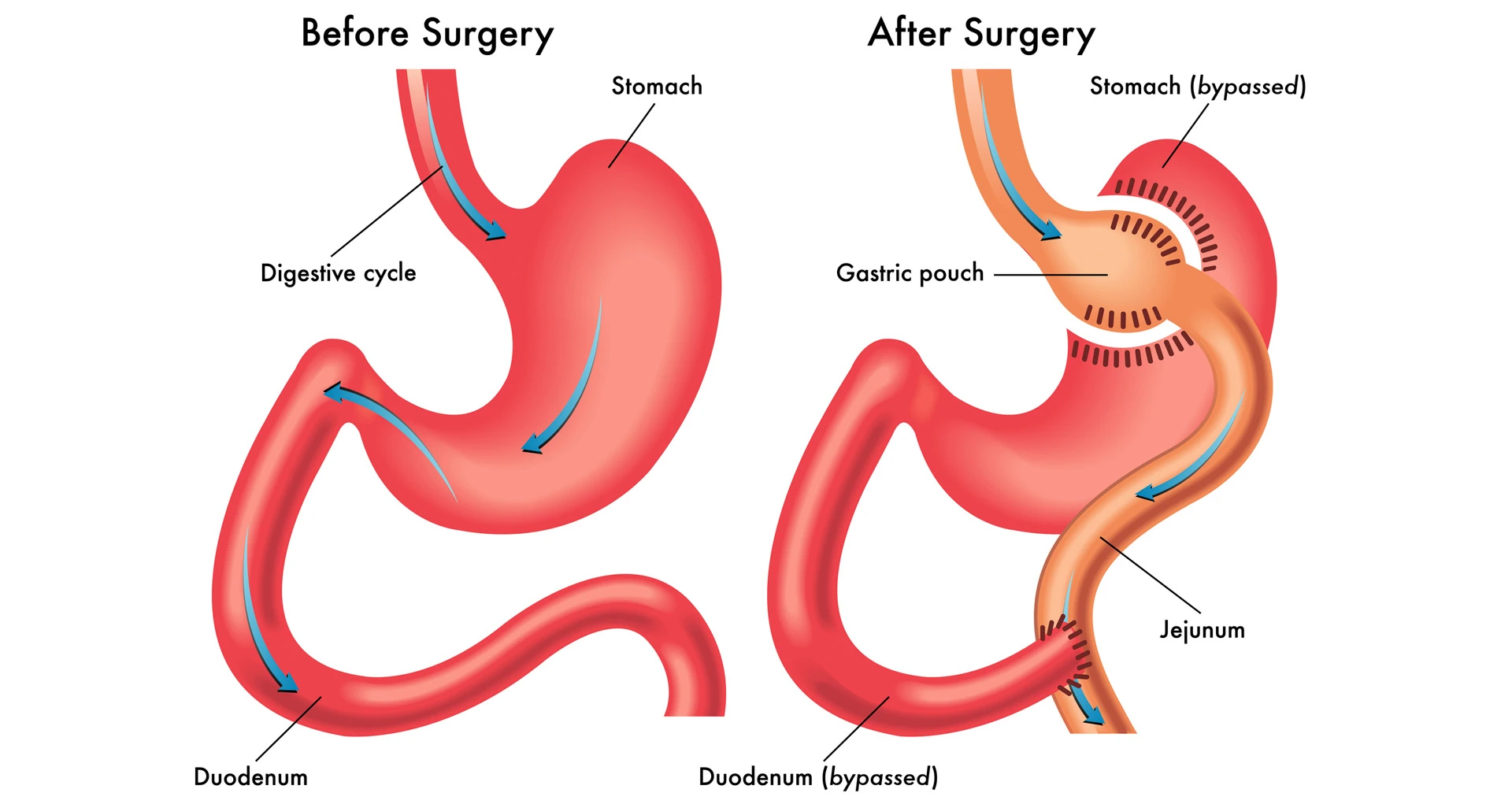
What happens to your body after gastric bypass extends beyond weight loss. The procedure creates hormonal changes that reduce hunger sensations and improve satiety. The digestive system undergoes significant adaptation during the first 18 months post-surgery, establishing new nutrient absorption patterns.
| Success Metric | Mini Gastric Bypass | Traditional Bypass |
|---|---|---|
| Weight Loss (1 year) | 70-80% EWL | 65-75% EWL |
| Operative Time | 45-60 minutes | 90-120 minutes |
| Type 2 Diabetes Resolution | 85% | 80% |
| Reduction in Medication Use | 76% | 70% |
| Satisfaction Rate | 92% | 85% |
The table demonstrates that mini gastric bypass results often surpass traditional bypass outcomes in several key metrics. Particularly noteworthy is the higher diabetes resolution rate and shorter operative time, which contributes to fewer anesthesia-related concerns.
How successful is a mini gastric bypass depends partly on patient selection and adherence to post-operative guidelines. Studies from leading bariatric centers report that 85-90% of patients achieve successful outcomes when properly screened and supported. The simplified anatomical configuration of the MGB contributes to its high success rate while maintaining effectiveness.
Patients report significant improvements in obesity-related conditions following MGB surgery. Joint pain reduction, sleep apnea improvement, and enhanced mobility typically occur within 3-6 months post-procedure. These quality-of-life improvements complement the weight loss outcomes and provide additional measures of success beyond the scale. While these benefits are encouraging, it is important to remain aware of potential Gastric Bypass Surgery Complications, as they can affect overall recovery and outcomes. Comprehensive post-operative care and regular follow-ups play crucial roles in minimizing these risks and ensuring long-term success.
Mini Gastric Bypass Surgery Risks and Long-Term Effects
The long-term effects of mini gastric bypass surgery present significant considerations for patients beyond the initial recovery period. Understanding these potential complications is essential for making informed decisions about this weight loss procedure.
- Nutritional Deficiencies: Mini gastric bypass can lead to severe vitamin and mineral deficiencies including B12, iron, calcium, vitamin D, and protein malabsorption.
- Bile Reflux Gastritis: One anastomosis gastric bypass complications often include bile reflux into the esophagus, causing chronic inflammation and discomfort.
- Marginal Ulcers: These painful ulcers develop at the connection between the stomach pouch and small intestine in approximately 5-10% of patients.
- Intestinal Obstruction: Late complications of mini gastric bypass may include bowel obstructions due to internal hernias or adhesions.
- Dumping Syndrome: This condition persists long-term in some patients, causing nausea, vomiting, and diarrhea after consuming high-sugar foods.
- Kidney Stones: The risk increases significantly after surgery due to altered mineral absorption.
- Bone Density Loss: Studies show accelerated bone mineral density reduction, increasing fracture risk over time.
- Weight Regain: Approximately 20-30% of patients experience significant weight regain within 5-10 years post-surgery.
| Mini Gastric Bypass Long-Term Complications | Prevalence | Typical Onset Time |
|---|---|---|
| Severe Malnutrition | 15-30% | 2+ years |
| Chronic Bile Reflux | 10-22% | 1-5 years |
| Marginal Ulcers | 5-10% | 1-3 years |
| Internal Hernias | 3-5% | 2-10 years |
| Bone Density Loss | 25-75% | 3+ years |
| Psychiatric Issues (depression, anxiety) | 20-30% | Variable |
This table illustrates the prevalence of major mini gastric bypass negative outcomes reported in clinical studies. Nutritional deficiencies remain the most common long-term complication, with malnutrition affecting up to 30% of patients beyond the two-year mark.
Gastric bypass complications years later can also manifest as metabolic issues. Hypoglycemia affects approximately 10-15% of patients several years post-surgery, causing dangerous blood sugar drops. Mini bypass risks extend to kidney function deterioration in some patients due to oxalate nephropathy.
What are the complications of gastric bypass 20 years later? Limited long-term data exists, but available research indicates increased risk of osteoporosis, potential need for revision surgery, and ongoing nutritional challenges. Complications 15 years after gastric bypass may include chronic anemia resistant to oral supplementation.
The disadvantages of mini gastric bypass also include psychological aspects. Many patients experience changes in alcohol tolerance, with some developing alcohol use disorders years after surgery. Additionally, the one anastomosis gastric bypass risks include potentially irreversible metabolic alterations that require lifelong medical monitoring.
Patients considering this procedure should weigh these mini bypass long-term complications against potential benefits and explore all treatment options with qualified medical professionals.
Early Post-Operative Complications of Mini Gastric Bypass
Mini gastric bypass surgery, while effective for weight loss, is associated with several post-operative complications that patients should be aware of. These complications typically appear within the first few weeks after surgery and require prompt attention from healthcare providers.
Common immediate complications after mini gastric bypass include:
- Bleeding (mini bypass bleeding) – Occurs in approximately 1-5% of patients, manifesting as hematemesis, melena, or tachycardia
- Infection (mini bypass infection) – Can develop at incision sites or internally, accompanied by fever, redness, and increased pain
- Anastomotic leaks – A serious complication occurring in 1-2% of cases, presenting with severe abdominal pain and fever
- Post-operative pain – Varying intensity of mini bypass post-operative pain that may persist for several days to weeks
- Nausea and vomiting – Common in the immediate recovery period, potentially leading to dehydration
- Deep vein thrombosis – Formation of blood clots in the legs with risk of pulmonary embolism
The early complications of mini gastric bypass require specific management approaches depending on their severity and presentation. Healthcare professionals typically follow these steps when addressing postoperative complications:
- Assessment of bleeding sources – Endoscopic evaluation is performed to identify and potentially treat the source of mini bypass bleeding
- Infection management – Treatment of infection after mini gastric bypass typically involves appropriate antibiotics and sometimes drainage procedures
- Pain control protocols – Structured medication regimens to address mini bypass post-operative pain while minimizing narcotic dependency
- Fluid and electrolyte maintenance – Critical for preventing dehydration, particularly important during mini bypass recovery problems
- Nutritional support – Modified intake strategies to support healing while adhering to post-surgical dietary restrictions
Healthcare professionals monitor patients closely for signs of early complications of mini gastric bypass, particularly during the first 72 hours. The clinical team maintains vigilance for subtle indications of postoperative complications gastric bypass patients might experience, such as tachycardia or unexplained pain that could signal internal bleeding or infection.
Patients experiencing mini bypass recovery problems should immediately report symptoms such as fever over 101.5°F (38.6°C), severe pain unrelieved by medication, persistent vomiting, or drainage from incision sites. Early intervention significantly reduces the risk of complications progressing to more serious conditions requiring surgical revision or prolonged hospitalization.
General Bariatric Surgery Complications
Bariatric surgery complications vary in severity and timing, with some appearing immediately after surgery while others may develop years later. Understanding these potential risks is essential for patients considering weight loss surgery options.
- Surgical complications include bleeding, infection, anastomotic leak, and bowel obstruction which occur in 5-10% of bariatric procedures
- Nutritional deficiencies affect up to 50% of patients following Roux-en-Y gastric bypass and other malabsorptive procedures
- Dumping syndrome occurs in approximately 20% of gastric bypass patients when food moves too quickly from stomach to intestines
- Internal hernias represent a serious late complication of bariatric surgery requiring emergency intervention
- Gallstone formation affects up to 35% of patients during rapid weight loss phases
Metabolic and physiological complications after bariatric surgery require ongoing monitoring and intervention. Roux-en-Y gastric bypass complications include more severe nutritional concerns than restrictive procedures, while all weight loss surgery complications need specialized management approaches.
| Complication Type | Sleeve Gastrectomy | Roux-en-Y Gastric Bypass | Biliopancreatic Diversion |
|---|---|---|---|
| Leak Rate | 1-2.4% | 0.8-2% | 0.7-4% |
| Nutritional Deficiencies | Moderate | Significant | Severe |
| Dumping Syndrome | Rare | Common (20-50%) | Common |
| GERD | May worsen | Usually improves | Usually improves |
| Mortality Risk | 0.1-0.5% | 0.1-0.5% | 0.5-1.1% |
This comparative data highlights that each bariatric procedure presents distinct complications profiles. Gastric bypass adverse events tend to include more metabolic disruptions, while restrictive procedures carry fewer nutritional risks but may present other complications. The rate of late complications of bariatric surgery increases with more complex procedures, particularly those with malabsorptive components like biliopancreatic diversion.
Proper patient education, surgical expertise, and lifelong follow-up represent the cornerstone of successful complication management in metabolic surgery. Weight loss surgery complications can be minimized through comprehensive pre-operative assessment and dedicated post-operative care protocols.