Breast surgery, encompassing procedures from augmentation to mastectomy, frequently leaves a visible reminder: the scar. While all surgical incisions result in some form of scar tissue, the appearance and evolution of these scars can vary significantly. Factors such as surgical technique, patient skin type, and post-operative care demonstrably influence the final cosmetic outcome. Understanding these distinctions is crucial for both practitioners and patients alike. Despite advancements in surgical methods and wound management, the inherent biological processes of healing lead to a diverse array of scar characteristics. This variability, often underestimated, directly impacts patient satisfaction and long-term well-being.
Table of Contents
What Different Breast Surgery Scars Look Like and Why They Vary
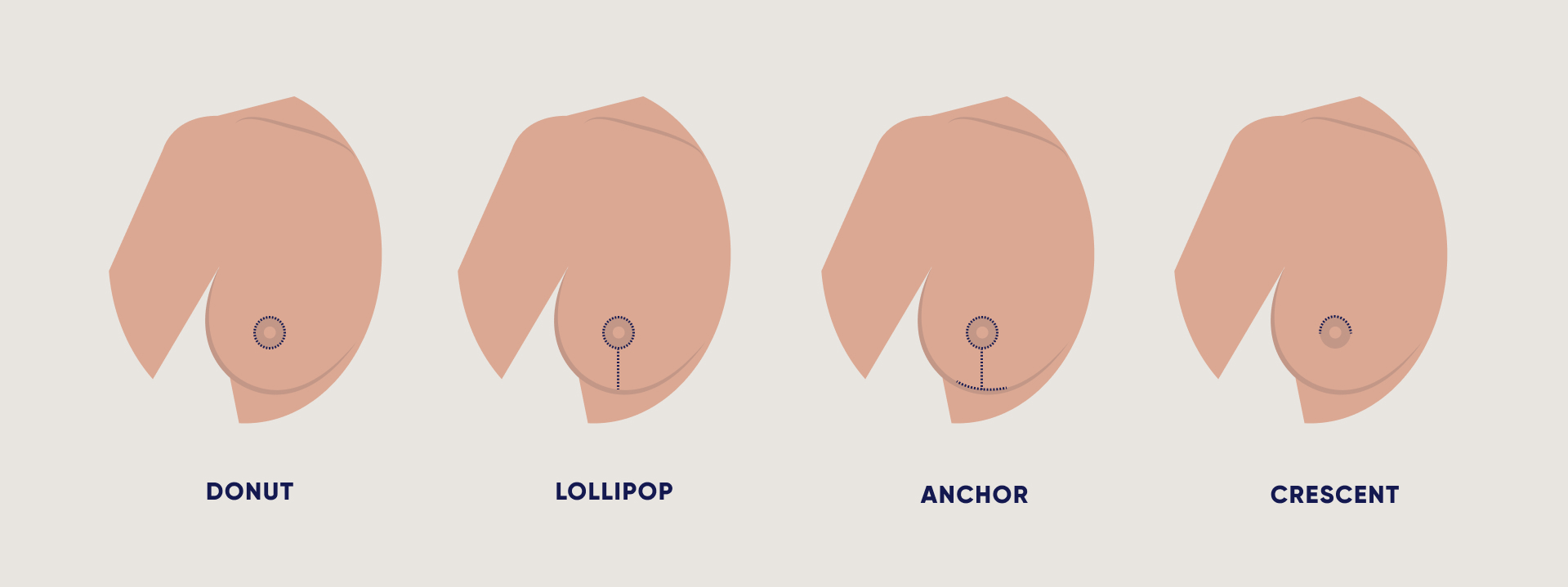
Breast augmentation scar types depend significantly on the surgical approach chosen by your surgeon. Inframammary scars appear as horizontal lines beneath the breast crease, typically measuring 4-6 centimetres in length. These incisions create the most predictable healing patterns and remain well-concealed within the natural breast fold. Periareolar scars form around the nipple-areola complex, appearing as circular or semi-circular marks that blend with the natural colour transition between areolar and breast skin.
Scarring on breast tissue varies dramatically based on the surgical procedure performed. Mastectomy scars present as diagonal or horizontal lines across the chest wall, often extending from the sternum towards the armpit. These scars typically measure 10-15 centimetres and may appear raised or depressed compared to surrounding skin. Scars after breast cancer surgery frequently include additional markings from lymph node removal, creating secondary incision lines in the underarm area.
The appearance of what do breast surgery scars look like changes substantially based on individual factors. Patients with darker skin tones often develop more prominent scarring due to increased melanin production during healing. Younger patients typically demonstrate better collagen synthesis, resulting in flatter, less noticeable scars. Genetic predisposition plays a crucial role, with some individuals naturally producing excessive scar tissue regardless of surgical technique.
Differences of scars after breast surgery become apparent when comparing various procedures. Breast reduction creates anchor-shaped scarring patterns, combining vertical incisions from nipple to breast crease with horizontal scars along the inframammary fold. Breast lift procedures produce similar patterns but with varying lengths depending on the degree of lifting required. These complex scar formations require longer healing periods compared to single-incision procedures.
Abnormal scarring presents distinct characteristics that distinguish it from normal healing. Hypertrophic scars appear thick, raised, and red, remaining within the original incision boundaries. Keloid scars extend beyond the initial wound margins, creating irregular, rope-like formations that may continue growing months after surgery. These problematic scars occur more frequently in individuals with African, Asian, or Hispanic heritage.
Breast scar appearance over time follows predictable phases of maturation. Initial inflammatory responses create red, swollen marks that gradually fade to pink within 3-6 months. Mature scars develop pale, flat appearances after 12-18 months of healing. Environmental factors, sun exposure, and mechanical stress influence final scar quality, with protected incisions typically achieving superior cosmetic outcomes compared to exposed areas. Breast Fat Transfer After 5 Years can reveal significant differences of scars after breast surgery, highlighting the quality of the wound healing process. Furthermore, patient care practices post-surgery play a crucial role in determining the long-term appearance of these scars.
Understanding the Breast Surgery Scar Healing Timeline
The breast scar healing process follows a predictable timeline that varies significantly depending on the surgical technique employed. Following breast augmentation, reduction, or lift procedures, patients typically observe initial wound closure within 7-10 days, whilst complete scar maturation extends considerably longer. Understanding how long for breast surgery scars to fade requires recognising that healing occurs in distinct phases.
During the inflammatory phase, lasting approximately 2-3 weeks, incision sites appear red and slightly raised. The proliferative phase follows, spanning 3-6 weeks, where collagen production increases substantially. This period determines how breast scars heal and influences long-term aesthetic outcomes. Patients frequently inquire about how long does it take for breast surgery scars to heal completely, expecting visible improvements within months.
Breast reduction scars after 6 months typically demonstrate significant colour fading and reduced elevation. The remodelling phase, commencing around week six, continues for 12-24 months. During this extended period, scars gradually soften, flatten, and approach the surrounding skin tone. How long do breast surgery scars take to heal depends largely on individual factors including age, skin type, and adherence to post-operative protocols.
Healed one year breast lift scars represent the gold standard for assessing surgical outcomes. At this milestone, most patients observe 80-90% of final scar maturation. The remaining refinement continues subtly over the subsequent year. How long do scars take to heal after breast augmentation follows similar patterns, though inframammary fold incisions typically heal more favourably than periareolar approaches.
The formation of scar tissue represents the body’s natural healing response. How long does scar tissue last after breast surgery varies considerably between individuals. Hypertrophic scarring may persist longer, requiring 18-24 months for optimal resolution. Regular follow-up appointments enable surgeons to monitor progression and identify patients requiring additional intervention. Understanding these timelines helps establish realistic expectations whilst ensuring optimal healing conditions throughout the recovery period.
Essential Tips for Post-Surgery Scar Care and Management
- Silicone gel sheeting represents the gold standard for breast surgery scar removal, with clinical studies demonstrating 86% improvement in scar appearance when used consistently for 12-24 hours daily over 2-3 months.
- Apply medical-grade silicone gel directly to scars around nipples twice daily, ensuring complete coverage of the affected area whilst maintaining proper hygiene protocols throughout the healing process.
- Massage therapy using circular motions helps break down scar tissue after breast surgery, improving flexibility and reducing adhesions when performed for 5-10 minutes twice daily after initial wound healing.
- Protect healing incisions from UV exposure using SPF 30 or higher sunscreen, as sun damage can cause permanent hyperpigmentation and worsen the appearance of surgical scars following breast reconstruction.
- Steroid injections administered by qualified practitioners effectively treat hypertrophic and keloid scars, with triamcinolone acetonide showing 70% success rates in reducing scar elevation and improving texture.
- Maintain optimal wound moisture using physician-recommended ointments during the initial healing phase, as dry wounds heal 40% slower and produce more prominent scarring than properly hydrated tissue.
- Begin scar management protocols within 2-3 weeks post-surgery once sutures are removed and wounds have achieved primary closure, as early intervention significantly improves long-term outcomes.
- Laser therapy including fractional CO2 and pulsed dye lasers effectively address bad breast implant scars by stimulating collagen remodelling and reducing erythema over 3-6 treatment sessions.
- Avoid tension and stretching of healing incisions by wearing properly fitted surgical bras and limiting overhead arm movements during the first 6-8 weeks following surgery.
- Topical treatments containing onion extract, vitamin E, and hyaluronic acid show moderate efficacy in caring for breast scars when applied consistently over extended periods.
- Schedule regular follow-up appointments to monitor scar progression and adjust treatment protocols, as professional assessment ensures optimal healing and early intervention for problematic scarring.
- Consider surgical scar revision for mature scars that remain raised, widened, or aesthetically concerning after 12-18 months of conservative management approaches.
- Compression therapy using medical-grade garments helps flatten and soften scars whilst improving circulation to the healing tissue, particularly effective for larger surgical sites.
- Document scar progression through clinical photography to track improvement and guide treatment decisions, enabling objective assessment of various intervention effectiveness.
- Nutritional support including adequate protein intake, vitamin C supplementation, and proper hydration facilitates optimal collagen synthesis and supports the natural healing process throughout recovery.
Comparing Minimally Invasive vs. Traditional Surgical Scars
The choice between minimally invasive and traditional surgical approaches significantly impacts scar formation patterns and long-term aesthetic outcomes in breast surgery procedures. Understanding these differences enables patients to make informed decisions regarding their surgical options.
| Comparison Criteria | Minimally Invasive Techniques | Traditional Surgical Approaches |
|---|---|---|
| Incision Length | 2-4 cm typically | 8-15 cm depending on procedure |
| Scar Placement | Hidden locations (axilla, areola border) | More visible areas (inframammary fold, vertical) |
| Initial Healing Time | 7-10 days for surface closure | 14-21 days for complete closure |
| Tissue Trauma | Minimal surrounding damage | Extensive soft tissue disruption |
| Long-term Appearance | Fine linear marks, often barely visible | More prominent, wider scars possible |
| Hypertrophic Risk | Significantly reduced | Higher probability of raised scarring |
Endoscopic breast augmentation techniques utilise small periareolar or transaxillary incisions, resulting in concealed scar placement that becomes virtually imperceptible over time. These approaches preserve the natural breast anatomy whilst minimising surgical trauma to surrounding tissues.
Traditional open surgical methods necessitate larger incisions to accommodate direct visualisation and instrument access. The inframammary fold approach, whilst providing excellent surgical exposure, creates more substantial scarring that requires extended healing periods and comprehensive aftercare protocols.
Wound tension distribution differs markedly between approaches. Minimally invasive techniques distribute mechanical stress across smaller tissue areas, promoting more favourable collagen remodelling and reducing the likelihood of keloid formation. Traditional methods often create higher tension concentrations at suture lines, potentially leading to wider, more noticeable scarring.
The vascular compromise associated with extensive tissue dissection in traditional approaches can impede optimal healing responses. Minimally invasive procedures preserve local blood supply more effectively, supporting enhanced tissue regeneration and superior aesthetic outcomes through improved cellular metabolism and oxygen delivery to healing tissues.
Can Breast Surgery Scars Be Revised or Improved?
Scar revision surgery represents the most comprehensive approach to improving unsatisfactory breast surgery scars. This surgical technique involves excising the existing scar tissue and creating a new, more aesthetically pleasing incision line. The procedure typically employs advanced suturing techniques, including layered closure methods and precise tissue approximation to minimise tension on the wound edges. Z-plasty and W-plasty techniques prove particularly effective for addressing contracted or widened scars, as these methods redistribute tension across multiple vectors rather than a single line.
Non-surgical treatments offer excellent alternatives for patients seeking scar improvement without additional surgery. Laser therapy, particularly fractional CO2 and pulsed dye lasers, effectively targets scar tissue by stimulating collagen remodelling and reducing erythema. These treatments work by creating controlled microscopic injuries that trigger the body’s natural healing response, gradually improving scar texture and colour. Steroid injections demonstrate remarkable efficacy in treating hypertrophic scars, with triamcinolone acetonide being the gold standard for reducing scar elevation and associated symptoms.
Radiofrequency treatments and microneedling procedures provide additional non-invasive options for scar enhancement. Radiofrequency energy penetrates deep into the dermis, heating tissue to promote collagen synthesis and tissue remodelling. Microneedling creates controlled micro-injuries that stimulate natural healing processes, particularly effective when combined with platelet-rich plasma or growth factor serums.
Topical treatments complement both surgical and non-surgical approaches to scar management. Silicone gel sheeting remains the evidence-based standard for scar treatment, demonstrating consistent results in improving scar appearance through hydration and pressure application. Professional-grade tretinoin creams accelerate cellular turnover, whilst vitamin E and onion extract preparations show moderate benefits in scar texture improvement.
Combination therapy approaches frequently yield superior results compared to single-modality treatments. Sequential treatment protocols might involve initial laser therapy followed by topical management, or surgical revision combined with post-operative laser treatments. The timing of interventions proves critical, with most revision procedures recommended after the initial healing period of twelve to eighteen months. Patient selection criteriainclude realistic expectations, adequate healing from the original surgery, and absence of ongoing complications that might compromise revision outcomes.
Psychological Impact of Different Scar Types and Coping Strategies
Surgical scarring significantly affects patients’ psychological wellbeing, with studies indicating that 75% of breast surgery patients experience some degree of emotional distress related to visible scarring. The psychological impact varies considerably based on scar location, size, and individual patient factors including age, pre-existing body image concerns, and social support systems.
Hypertrophic scars and keloid formations typically generate the most substantial psychological burden due to their raised, discoloured appearance and potential for continued growth. Our clinical experience demonstrates that patients with these scar types report higher levels of body dysmorphia and social anxiety. Conversely, mature linear scars that fade to skin tone generally produce less psychological distress, though individual responses remain highly variable.
Effective coping strategies encompass both psychological and practical approaches:
- Cognitive behavioural therapy specifically targeting body image concerns proves highly effective in reducing scar-related distress
- Mindfulness techniques and acceptance-based interventions help patients develop healthier relationships with their changed appearance
- Gradual exposure therapy assists patients in rebuilding confidence in social situations
- Support group participation provides peer validation and shared coping experiences
- Scar massage therapy offers both physical benefits and psychological empowerment through active self-care
- Clothing adaptation strategies enable patients to feel comfortable whilst adjusting to their new appearance
Professional counselling becomes essential when patients exhibit persistent avoidance behaviours, relationship difficulties, or symptoms of clinical depression. Research indicates that early psychological intervention within the first three months post-surgery significantly improves long-term adjustment outcomes.
The multidisciplinary approach we employ recognises that effective scar management extends beyond physical healing. Integrating psychological support with surgical expertise creates comprehensive care pathways that address both aesthetic concerns and emotional wellbeing. Patients who receive coordinated psychological support alongside their surgical treatment demonstrate improved satisfaction rates and better overall quality of life outcomes, emphasising the critical importance of addressing the complete spectrum of scarring impacts.