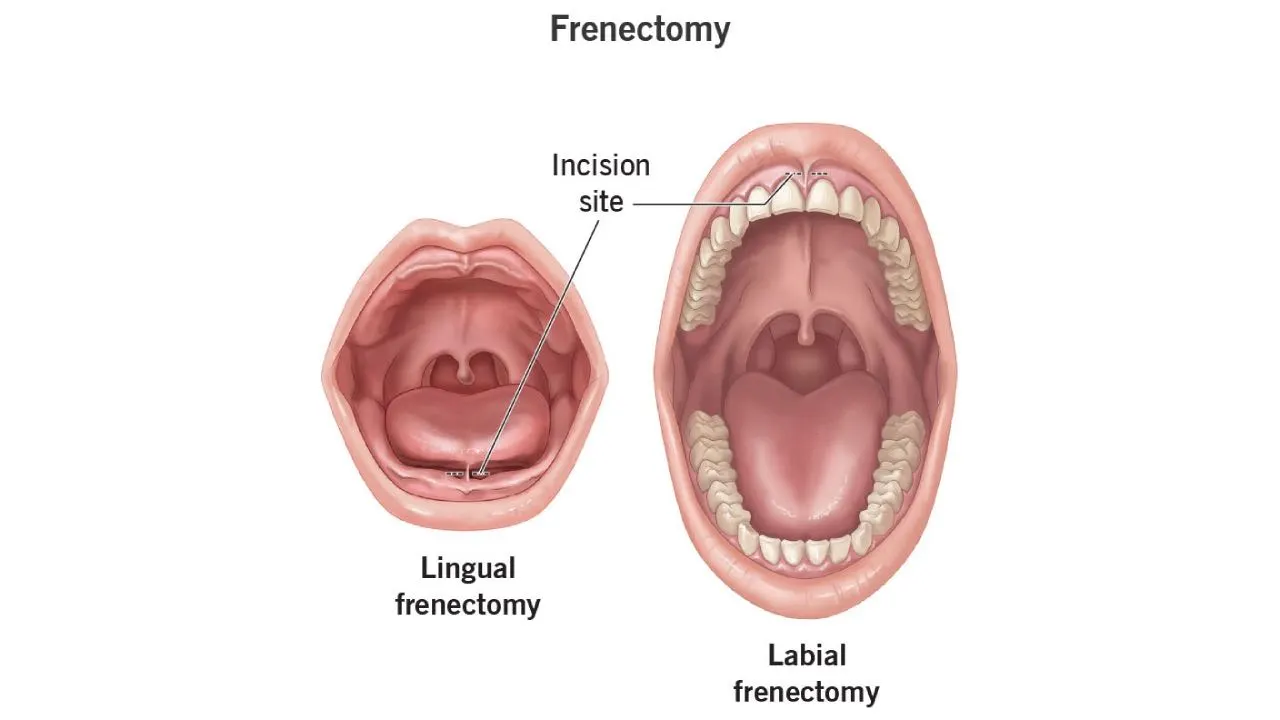
A frenectomy is a surgical procedure, often performed by dental professionals. It involves the removal or reduction of a frenum, a small fold of tissue. This tissue connects two parts, limiting the movement of one. For instance, a labial frenum connects the lip to the gum. A lingual frenum connects the tongue to the floor of the mouth. The presence of an overly restrictive frenum can lead to various oral health concerns. These issues may include difficulty with speech, eating, or even orthodontic problems. Clinical observations consistently link specific frenum anomalies to impaired oral function. For example, a prominent labial frenum may cause a gap between front teeth. Similarly, a short lingual frenum, known as ankyloglossia, can restrict tongue mobility. This restriction often impacts breastfeeding in infants and speech articulation in children. Therefore, understanding the anatomical variations and potential implications of frenula is crucial for effective diagnosis and intervention. The decision to perform a frenectomy is based on a thorough clinical assessment. This assessment evaluates the frenum’s attachment, size, and its impact on oral function. Such procedures are well-established within modern dentistry. Their efficacy in resolving related oral issues is supported by extensive clinical data.
Table of Contents
What is a Frenectomy and How Does it Work?
A frenectomy is a surgical procedure that removes or modifies the frenum, a small band of tissue that connects the lips, tongue, or cheeks to the gums. This oral surgery frenectomy addresses anatomical restrictions that can interfere with normal oral function, speech development, and dental health.
Types of Frenectomy Procedures
The procedure targets specific anatomical locations where restrictive tissue bands create functional limitations:
- Lingual frenectomy addresses tongue tie conditions by modifying the tissue connecting the tongue to the floor of the mouth
- Labial frenectomy involves removing or adjusting the frenum that connects the lips to the gums
- Upper lip frenectomy targets the tissue band between the upper lip and gums, often improving gum health and smile aesthetics
- Lower lip frenectomy addresses restrictions in the lower labial area that can affect speech and oral hygiene
Understanding Frenectomy Meaning and Clinical Indications
The frenectomy meaning encompasses both functional and aesthetic improvements in oral health. Clinical evidence demonstrates that restrictive frena can cause significant complications including diastema formation, periodontal problems, and speech impediments. Research indicates that frenectomy tongue tie procedures show success rates exceeding 90% in improving tongue mobility and reducing associated symptoms.
Frenectomy lip tie conditions particularly affect infants and young children, where tight labial frena can interfere with breastfeeding and proper oral development. Studies from UK dental practices report that early intervention through frenectomy procedure protocols leads to better long-term outcomes in speech development and dental alignment.
Anatomical Considerations and Patient Assessment
The frenectomy dental evaluation process involves comprehensive assessment of tissue attachment levels, mobility restrictions, and functional impact. Clinicians examine the degree of tissue tension, gingival recession patterns, and interference with normal oral functions. Labial frenectomy before and after smile assessments demonstrate measurable improvements in both functional capacity and aesthetic outcomes.
Upper labial frena particularly influence smile dynamics and gingival health. When these tissues create excessive tension, they can contribute to midline diastema formation and compromise periodontal stability. The upper lip frenectomy addresses these concerns by releasing restrictive tissue bands and allowing natural tissue repositioning.
Tissue Healing and Recovery Expectations
Post-operative healing following frenectomy procedures typically occurs within 7-14 days for most patients. The surgical site undergoes predictable healing phases, with initial tissue adaptation occurring within 48-72 hours. UK clinical guidelines recommend specific post-operative care protocols that optimise healing outcomes and minimise complications.
Lingual frenectomy recovery often shows immediate functional improvements, with patients reporting enhanced tongue mobility within the first week. The tissue remodelling process continues for several weeks, with final functional outcomes typically achieved within 4-6 weeks post-operatively.
The procedure’s effectiveness depends on accurate diagnosis, appropriate surgical planning, and comprehensive post-operative care. Contemporary frenectomy procedure techniques emphasise minimal tissue trauma whilst achieving optimal functional outcomes for patients across all age groups.
Step-by-Step Surgical Methods and Techniques
Precise execution of frenectomy procedures requires mastery of multiple surgical approaches and comprehensive understanding of anatomical considerations. Each technique offers distinct advantages depending on patient presentation and clinical requirements.
Traditional Surgical Frenectomy Techniques
The conventional scalpel approach remains the gold standard for many oral and maxillofacial surgeons performing frenectomy procedures:
- Local anaesthesia administration using lidocaine with epinephrine in the target area
- Tissue stabilisation with forceps or haemostats to secure the frenum
- Incision placement at the base of the frenum using a sharp scalpel blade
- Blunt dissection to separate muscle fibres from underlying periosteum
- Haemostasis achievement through electrocautery or direct pressure application
- Wound closure with resorbable sutures when indicated
- Pressure application for final bleeding control
Key advantages of traditional frenectomy procedure steps include:
- Excellent visualisation of anatomical structures throughout the procedure
- Precise tissue control allowing careful dissection of muscle attachments
- Cost-effective approach with minimal equipment requirements
- Proven track record with decades of successful clinical outcomes
- Versatile application across various patient age groups and presentations
Laser-Assisted Frenectomy Techniques
Laser frenectomy procedures utilise diode or CO2 laser technology for precise tissue ablation:
- Laser calibration with appropriate power settings based on tissue thickness
- Safety protocols including eye protection for patient and surgical team
- Tissue engagement using focused laser beam at frenum attachment site
- Controlled ablation with systematic tissue removal in layers
- Immediate coagulation of blood vessels during cutting process
- Tissue inspection to ensure complete frenum release
- Final assessment of wound margins and bleeding control
Primary benefits of laser-assisted techniques include:
- Reduced bleeding due to simultaneous vessel coagulation
- Minimal post-operative discomfort compared to traditional methods
- Faster healing times with reduced inflammatory response
- Enhanced precision in tissue removal and contouring
- Reduced need for sutures in many clinical scenarios
- Excellent patient acceptance due to reduced trauma
Post-Operative Care and Recovery Protocols
Comprehensive post-operative management ensures optimal healing outcomes:
- Pain management with prescribed analgesics and anti-inflammatory medications
- Oral hygiene modifications including gentle brushing and chlorhexidine rinses
- Dietary restrictions emphasising soft foods for initial healing period
- Activity limitations avoiding strenuous physical exercise for 48-72 hours
- Ice application during first 24 hours to minimise swelling
- Wound monitoring for signs of infection or delayed healing
Potential Complications and Management Strategies
Recognition and prompt management of complications ensures successful outcomes:
- Excessive bleeding managed through direct pressure and vasoconstrictor application
- Infection prevention using prophylactic antibiotics when indicated
- Scar formation minimised through proper surgical technique and follow-up care
- Incomplete release addressed through revision procedures if necessary
- Nerve damage prevented through careful anatomical identification during surgery
Follow-up and Long-Term Outcomes
Systematic follow-up protocols typically include appointments at one week, one month, and three months post-operatively. Patients demonstrate significant improvements in oral function, speech articulation, and feeding capabilities within the first month following surgery. Long-term success rates exceed 95% when proper surgical technique and post-operative care protocols are followed. Functional assessments reveal sustained improvements in tongue mobility, lip function, and overall oral hygiene maintenance throughout the healing period.
Finding Treatment and Healthcare Access
Accessing frenectomy NHS adults treatment begins with consulting your general practitioner, who will assess your condition and determine the medical necessity. NHS funding typically covers procedures that significantly impact speech, oral hygiene, or cause recurrent dental problems in adults.
- Schedule an initial consultation with your GP to discuss symptoms and functional limitations caused by restrictive frenums
- Obtain a referral to an oral and maxillofacial surgeon or periodontist within the NHS system
- Attend the specialist assessment where clinical examination and treatment planning occur
- Receive treatment scheduling based on clinical priority and local NHS waiting times
- Complete pre-operative requirements including medical history review and consent procedures
NHS trusts across England, Scotland, Wales, and Northern Ireland provide frenectomy UK services through their oral surgery departments. However, availability and waiting times vary significantly between regions, with some areas experiencing delays of several months for non-urgent cases.
When searching for frenectomy near me, adults should consider both NHS and private healthcare options. Private treatment offers faster access but requires significant financial investment, typically ranging from £200 to £800 depending on complexity and location.
Adult patients seeking frenectomy procedures face specific considerations that differ from pediatric cases:
- Medical complexity increases with age, requiring comprehensive cardiovascular and medication assessments
- Healing processes may be slower compared to younger patients, necessitating extended recovery periods
- Functional expectations must be realistic, as adult tissue adaptation differs from childhood development
- Orthodontic coordination often becomes necessary when addressing tongue-tie or lip-tie restrictions
- Workplace considerations require planning for time off and dietary modifications during recovery
Frenectomy in adults demonstrates excellent success rates when performed by qualified oral surgeons. Research indicates that 85-90% of adult patients experience significant improvement in targeted symptoms within six months post-procedure. However, adult outcomes depend heavily on pre-existing tissue changes and patient compliance with post-operative care protocols.
Regional NHS dental services maintain databases of qualified providers, ensuring patients receive care from appropriately trained specialists. Many NHS trusts now offer multidisciplinary clinics where oral surgeons collaborate with speech therapists and orthodontists to optimize treatment outcomes.
Private healthcare networks across the UK provide expedited access to frenectomy procedures, often with same-week consultation availability. Insurance coverage varies, with some policies covering medically necessary procedures while excluding cosmetic improvements. Adults experiencing significant functional impairment should document symptoms thoroughly to support insurance claims and NHS referral processes, ensuring access to appropriate surgical intervention when conservative treatments prove insufficient.