Obesity presents a significant global health challenge, impacting millions worldwide. Its complex etiology involves genetic, environmental, and behavioral factors. This chronic disease elevates the risk of numerous comorbidities, including type 2 diabetes and cardiovascular disease. Traditional weight loss methods often yield limited long-term success for individuals with severe obesity. Bariatric surgery, particularly gastric sleeve surgery, has emerged as a highly effective intervention. This surgical approach demonstrably facilitates substantial and sustained weight reduction. It provides a crucial pathway for patients seeking significant improvements in their metabolic health. The procedure involves removing a large portion of the stomach. This restriction physically limits food intake and promotes satiety. Consequently, it fundamentally alters the physiological landscape of weight regulation.
Table of Contents
How Does a Smaller Stomach Lead to Weight Loss After a Gastric Sleeve?
Many patients understandably question how the vertical sleeve gastrectomy procedure achieves weight loss when existing body fat remains immediately after surgery. Understanding the post-surgical anatomy bariatric surgery creates provides clarity on this fundamental concern.
The Anatomical Transformation Process
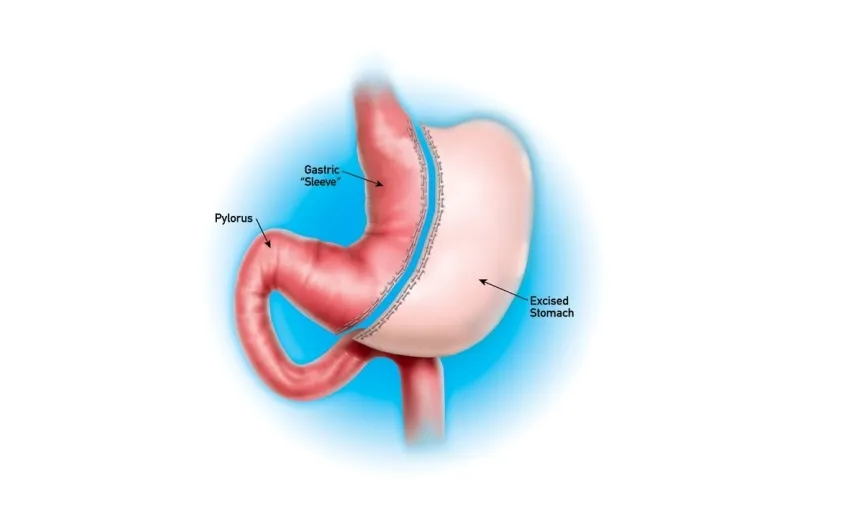
The sleeve gastrectomy procedure fundamentally alters digestive anatomy through specific steps:
- Stomach volume reduction from approximately 1,200ml to 100-150ml capacity
- Removal of the fundus – the stomach’s stretchy upper portion that accommodates large food volumes
- Creation of a narrow gastric sleeve resembling a banana shape along the lesser curvature
- Preservation of the pyloric valve maintaining normal stomach emptying mechanisms
This anatomy of gastric sleeve creates immediate physical restrictions that force portion control regardless of existing adipose tissue distribution.
Physical Mechanisms Behind Weight Reduction
The gastric sleeve real stomach operates through measurable capacity limitations. Research demonstrates that patients consume 60-80% fewer calories daily due to anatomical constraints rather than willpower alone.
Key physical changes include:
- Rapid satiety signals when the small pouch stretches
- Slower food transit allowing prolonged fullness sensation
- Reduced accommodation preventing volume expansion over time
- Earlier activation of stretch receptors triggering meal termination
Normal Anatomy After Gastric Sleeve: Capacity Comparison
The following table illustrates the dramatic anatomical differences:
| Measurement | Pre-Surgery | Post-Surgery |
|---|---|---|
| Stomach Capacity | 1,200ml | 100-150ml |
| Meal Volume | 500-800ml | 60-120ml |
| Eating Duration | 10-30 minutes | 20-45 minutes |
| Daily Caloric Intake | 2,000-4,000 | 600-1,200 |
The Weight Loss Timeline Through Anatomical Function
The postoperative anatomy gastric sleeve enables progressive fat utilisation through sustained caloric deficit. When daily intake drops to 800-1,200 calories whilst metabolic demands remain at 1,800-2,500 calories, the body mobilises stored adipose tissue for energy.
This anatomy of weight loss with gastric sleeve surgery creates a deficit of 600-1,700 calories daily. Over months, this consistent gap forces the body to metabolise existing fat reserves systematically.
The smaller stomach serves as a permanent portion control mechanism, ensuring long-term caloric restriction without conscious dietary restraint. Patients lose weight because their modified anatomy prevents overconsumption, creating the sustained energy deficit necessary for adipose tissue reduction. The existing body fat gradually diminishes as the restricted gastric capacity maintains the caloric deficit essential for continued weight loss. This ongoing deficit is crucial for understanding the Gastric Sleeve Life-Changing Transformation within the anatomy of weight loss with gastric sleeve surgery. It significantly alters the digestive process, thereby aiding in effective weight management.
The Science Behind Hunger Reduction: Hormonal Effects of Gastric Sleeve
Gastric sleeve surgery triggers profound hormonal changes that fundamentally alter appetite regulation and metabolic processes. These biochemical modifications work synergistically with the physical stomach reduction to create sustainable weight loss outcomes.
Primary Hormonal Mechanisms
The procedure significantly impacts several key hormones responsible for hunger and satiety:
- Ghrelin reduction: Removal of the gastric fundus eliminates approximately 70-80% of ghrelin-producing cells, dramatically decreasing this primary hunger hormone
- GLP-1 enhancement: Increased glucagon-like peptide-1 production improves insulin sensitivity and promotes satiety signals to the brain
- PYY elevation: Peptide YY levels rise substantially, creating prolonged feelings of fullness after meals
- Leptin optimization: Enhanced leptin sensitivity allows for better recognition of energy storage signals
- Insulin regulation: Improved insulin function reduces blood glucose fluctuations that trigger hunger episodes
Hormonal Response Comparison
The following data demonstrates the dramatic hormonal shifts patients experience:
| Hormone | Pre-Surgery Level | Post-Surgery Level | Impact on Appetite |
|---|---|---|---|
| Ghrelin | 600-800 pg/ml | 150-200 pg/ml | 75% hunger reduction |
| GLP-1 | 10-15 pmol/L | 25-35 pmol/L | Enhanced satiety |
| PYY | 20-30 pg/ml | 45-60 pg/ml | Prolonged fullness |
Metabolic Pathway Integration
These hormonal modifications create cascading effects throughout the endocrine system. The hypothalamic-pituitary axis receives altered signals, fundamentally reprogramming appetite control centres. Neuropeptide Y production decreases by 40-50%, while POMC neuron activity increases significantly.
The vagal nerve pathway also undergoes substantial changes, with reduced afferent signalling from the remaining stomach tissue. This neurohormonal integration ensures that hunger reduction persists beyond the initial recovery period.
Clinical evidence demonstrates that these hormonal adaptations maintain effectiveness for 5-10 years post-surgery, with ghrelin levels remaining consistently suppressed. The combination of reduced gastric capacity and optimized hormone production creates an environment where patients naturally consume appropriate portions while experiencing genuine satisfaction from smaller meals.
Timeline of Physical Recovery: What to Expect Week by Week
Understanding the recovery timeline helps patients prepare mentally and physically for their bariatric surgery journey. Each phase brings distinct milestones and healing markers that guide the pathway to optimal recovery.
Immediate Post-Operative Period (Week 1)
- Surgical site healing begins immediately with initial wound closure and early tissue repair
- Patients experience controlled pain levels managed through prescribed analgesics and monitoring protocols
- Clear liquid diet remains the exclusive nutritional intake, with strict portion limitations
- Walking short distances becomes essential for preventing blood clots and promoting circulation
- Sleep patterns typically remain disrupted due to position restrictions and recovery discomfort
- Drainage tubes may remain in place for the first 24-48 hours post-surgery
- Daily weight monitoring starts immediately to track initial fluid losses
- Medical team conducts regular vital sign assessments and wound inspections
Early Recovery Phase (Weeks 2-4)
- Incision sites show significant improvement with reduced swelling and inflammatory responses
- Dietary progression advances to pureed foods following medical clearance and tolerance testing
- Physical activity increases gradually to include longer walking sessions and light household tasks
- Energy levels begin stabilising as the body adapts to new nutritional patterns
- Sleep quality improves markedly as surgical discomfort decreases substantially
- Follow-up appointments occur regularly to monitor healing progress and nutritional status
- Patients typically return to desk-based work activities during this recovery window
- Vitamin supplementation protocols become established and integrated into daily routines
Intermediate Recovery (Weeks 5-8)
- Surgical sites achieve near-complete healing with minimal visible scarring remaining
- Soft solid foods enter the dietary regimen following successful tolerance of previous stages
- Exercise capacity expands to include light resistance training and extended cardiovascular activities
- Digestive comfort increases significantly as the stomach adapts to modified anatomy
- Professional responsibilities resume fully for most patients during this timeframe
- Nutritional absorption patterns stabilise as the digestive system establishes new functioning rhythms
- Mental clarity and cognitive function return to pre-surgical baseline levels
- Social eating situations become manageable with proper portion control strategies
Long-Term Adaptation (After 2 Months)
- Complete tissue healing occurs with full restoration of normal wound strength parameters
- Regular textured foods integrate successfully into daily eating patterns with continued portion awareness
- Exercise tolerance reaches levels comparable to pre-surgical fitness capabilities
- Digestive processes function optimally with minimal discomfort or dietary restrictions
- Routine medical monitoring transitions to scheduled quarterly assessments rather than frequent check-ups
- Work performance and daily activities return to full capacity without surgical limitations
- Nutritional supplementation becomes a permanent lifestyle component requiring ongoing compliance
- Body composition changes become increasingly apparent as recovery stabilises completely
What Are the Long-Term Body Changes After Bariatric Surgery?
Bariatric surgery fundamentally alters the anatomy of human stomach and bariatric surgery procedures create permanent structural modifications that extend far beyond the initial recovery period. These anatomical changes trigger cascading physiological adaptations throughout the digestive system, affecting nutrient absorption, metabolic processes, and overall body composition for years following the procedure.
Understanding anatomy for bariatric surgery reveals that patients experience several ongoing physiological adaptations:
- Altered gastric emptying patterns that permanently change how food moves through the digestive tract
- Modified bile acid circulation affecting fat metabolism and glucose regulation
- Reduced intrinsic factor production leading to potential vitamin B12 deficiency
- Changes in gastric pH levels impacting mineral absorption, particularly iron and calcium
- Adaptations in intestinal villi structure enhancing nutrient uptake efficiency
Long-term complications require continuous monitoring throughout the patient’s lifetime. The long-term side effects of gastric sleeve procedures demonstrate that anatomical changes continue evolving years after surgery. Patients frequently develop dumping syndrome, characterized by rapid gastric emptying causing nausea, cramping, and diarrhea. Nutritional deficiencies become increasingly prevalent, with studies indicating that 75% of patients develop at least one deficiency within five years.
The following table summarizes critical long-term anatomical risks:
| Complication | Timeframe | Prevalence Rate |
|---|---|---|
| Gastric pouch stretching | 2-5 years | 35-40% |
| Stricture formation | 1-3 years | 15-20% |
| Marginal ulceration | 6 months-2 years | 8-12% |
Metabolic adaptations persist indefinitely, with patients experiencing permanent alterations in hunger and satiety hormone production. The reduced stomach capacity maintains weight loss effectiveness, though anatomical adaptations continue progressing throughout the patient’s lifetime. These sustained physiological changes underscore the importance of lifelong medical supervision and nutritional supplementation following bariatric procedures.