Diabetic retinopathy stands as a critical complication of diabetes, posing a significant threat to vision globally. This progressive eye disease, resulting from damage to the blood vessels of the light-sensitive tissue at the back of the eye (the retina), is a leading cause of blindness among working-aged adults. Early detection and timely intervention are paramount to preventing irreversible vision loss. This comprehensive guide will delineate the complexities of diabetic retinopathy, explore its diagnostic protocols, and provide an in-depth analysis of the various diabetic retinopathy treatment modalities available, offering clarity for patients seeking effective management and care.
Table of Contents
Understanding Diabetic Retinopathy
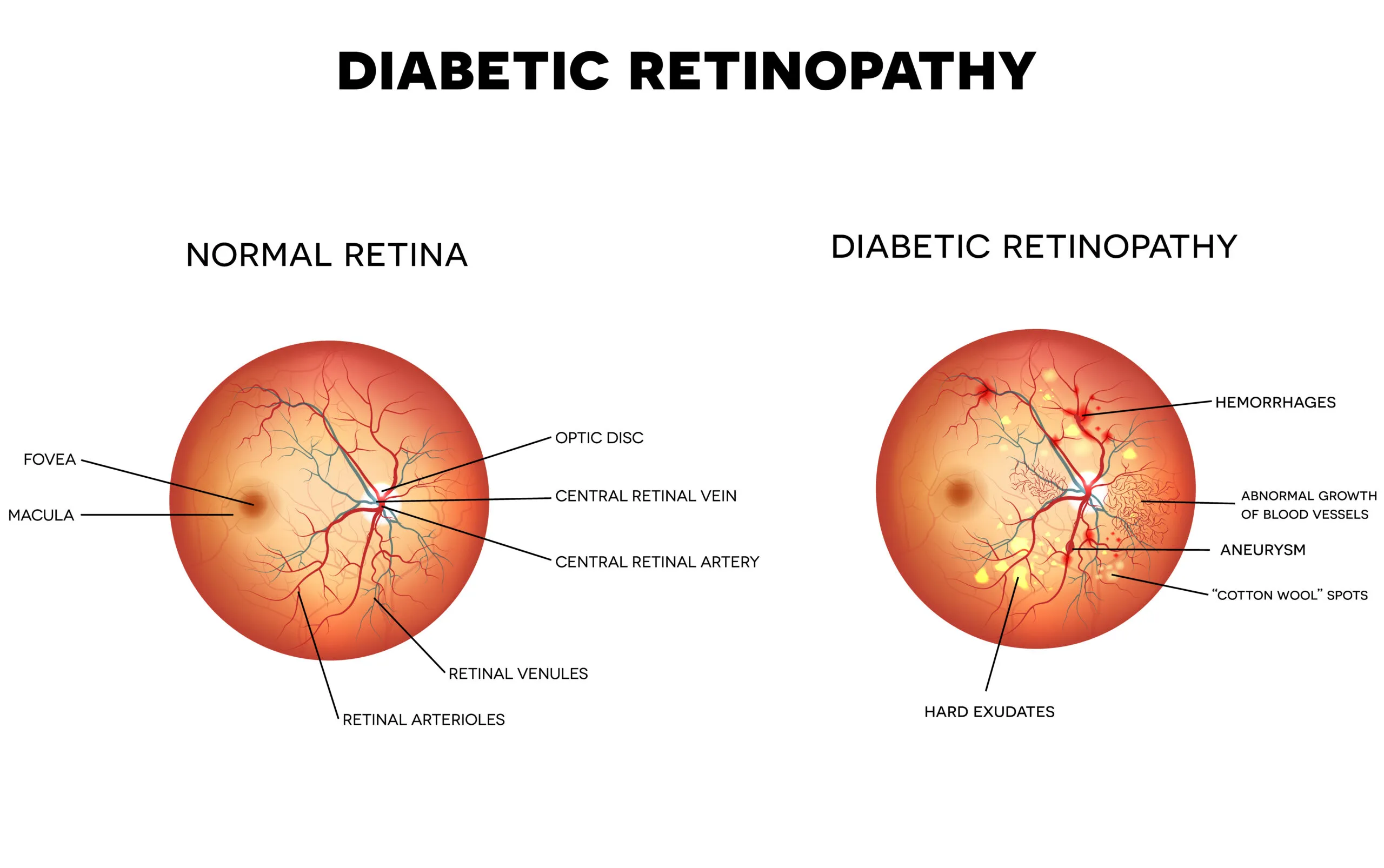
Diabetic retinopathy occurs when high blood sugar levels damage the tiny blood vessels that nourish the retina. Over time, these vessels can swell, leak fluid, or even close off completely, depriving the retina of essential blood supply. In advanced stages, new, abnormal blood vessels may grow on the retina’s surface, which can bleed into the eye or cause scar tissue to form, leading to retinal detachment and severe vision impairment.
Stages of Diabetic Retinopathy
Diabetic retinopathy progresses through distinct stages, each requiring specific attention and management:
- Non-Proliferative Diabetic Retinopathy (NPDR): This initial stage is characterized by microaneurysms (small bulges in blood vessels), hemorrhages, hard exudates (fat deposits), and macular edema (swelling of the macula, the central part of the retina responsible for sharp, detailed vision). Mild NPDR involves minimal changes, while moderate NPDR shows more widespread vascular abnormalities. Severe NPDR exhibits extensive damage, with numerous microaneurysms and hemorrhages, and often indicates a high risk of progression to the advanced stage.
- Proliferative Diabetic Retinopathy (PDR): This is the advanced stage of the disease, marked by the growth of new, fragile blood vessels (neovascularization) on the surface of the retina and optic nerve. These new vessels are prone to bleeding, leading to vitreous hemorrhage. Furthermore, the scar tissue that often accompanies these vessels can contract, pulling on the retina and causing tractional retinal detachment, a serious condition that can lead to permanent blindness if untreated.
Diagnostic Protocols for Diabetic Retinopathy
Accurate diagnosis is the cornerstone of effective diabetic retinopathy management. Regular, comprehensive eye examinations are crucial for all individuals with diabetes, regardless of their current vision status. These examinations allow ophthalmologists to detect the subtle signs of retinal damage before significant vision loss occurs, enabling timely intervention.
Key Diagnostic Procedures
- Dilated Eye Exam: During this examination, eye drops are used to widen the pupils, allowing the ophthalmologist a clear view of the retina and optic nerve. This visual inspection helps identify abnormal blood vessels, swelling, and other signs of diabetic retinopathy.
- Fluorescein Angiography (FA): A dye is injected into a vein in the arm, which travels to the blood vessels in the eye. A special camera then captures images as the dye passes through the retinal vessels, highlighting any leakage, blockages, or abnormal new vessels. This provides a detailed map of retinal vascular health.
- Optical Coherence Tomography (OCT): This non-invasive imaging technique uses light waves to create cross-sectional images of the retina. It is invaluable for detecting and monitoring macular edema, assessing retinal thickness, and identifying fluid accumulation within or under the retina, providing precise measurements that guide treatment decisions.
Advanced Diabetic Retinopathy Treatment Approaches
The primary goals of diabetic retinopathy treatment are to halt the progression of the disease, reduce existing damage, and preserve vision. The choice of treatment depends on the stage and severity of the retinopathy, as well as the presence of macular edema. Modern ophthalmology offers several highly effective therapeutic options.
Anti-VEGF Injections
Anti-vascular endothelial growth factor (anti-VEGF) medications are a revolutionary advancement in the treatment of diabetic macular edema (DME) and proliferative diabetic retinopathy (PDR). VEGF is a protein that stimulates the growth of new, abnormal blood vessels and increases fluid leakage in the retina. Anti-VEGF drugs block the action of this protein.
These medications are administered directly into the vitreous gel of the eye via a fine needle in a sterile outpatient procedure. Common anti-VEGF agents include ranibizumab (Lucentis), aflibercept (Eylea), and bevacizumab (Avastin). Studies have demonstrated that anti-VEGF therapy can significantly improve visual acuity and reduce macular edema in a substantial number of patients. A study published in the *New England Journal of Medicine* (The DRCR Network, 2015) found that anti-VEGF therapy was superior to laser photocoagulation for DME in terms of visual acuity outcomes, particularly in eyes with worse baseline vision. This research underscored the efficacy of these injections as a primary treatment for DME, highlighting their capacity to not only stabilize but often improve vision by diminishing swelling and inhibiting abnormal vessel growth.
Retinal Laser Treatment (Photocoagulation)
Laser photocoagulation has been a cornerstone of diabetic retinopathy treatment for decades and remains a vital option, particularly for PDR and certain cases of DME.
Panretinal Photocoagulation (PRP)
PRP, also known as scatter laser treatment, is primarily used for proliferative diabetic retinopathy. It involves applying numerous tiny laser burns to the peripheral retina, intentionally destroying areas of ischemic (oxygen-deprived) tissue. This reduces the retina’s demand for oxygen, thereby signaling the abnormal new blood vessels to regress. PRP helps to prevent vitreous hemorrhage and tractional retinal detachment. While effective in preventing severe vision loss, PRP can sometimes lead to some loss of peripheral vision, night vision, and color vision.
Focal/Grid Laser Treatment
This type of laser treatment is targeted specifically at diabetic macular edema. Focal laser involves precise application of laser burns to individual leaking microaneurysms near the macula, sealing them off. Grid laser treatment involves applying a pattern of light laser burns over areas of diffuse leakage or swelling in the macula. The aim is to reduce fluid leakage, stabilize vision, and prevent further deterioration. While less common as a primary treatment since the advent of anti-VEGF injections, it may still be used in conjunction with injections or for specific cases of DME.
Vitrectomy
Vitrectomy is a surgical procedure performed for advanced cases of proliferative diabetic retinopathy, where significant complications have occurred. This complex surgery is typically reserved for instances of non-clearing vitreous hemorrhage, tractional retinal detachment, or severe epiretinal membranes.
During a vitrectomy, the ophthalmologist removes the vitreous gel (the clear, jelly-like substance that fills the eye). This allows for the removal of blood, scar tissue, and any membranes that are pulling on the retina. In cases of retinal detachment, the retina is carefully reattached to the back of the eye. The vitreous gel is then replaced with a saline solution, gas, or silicone oil. Vitrectomy is a highly effective procedure for restoring vision in severe cases that would otherwise lead to permanent blindness, demonstrating the comprehensive range of treatments available for complex eye conditions.
Corticosteroids
Intravitreal corticosteroid injections, such as triamcinolone acetonide or sustained-release dexamethasone implants (Ozurdex), are another option for managing persistent diabetic macular edema, particularly in patients who do not respond adequately to anti-VEGF therapy or for whom anti-VEGF therapy is contraindicated. Corticosteroids work by reducing inflammation and fluid leakage. However, their use must be carefully weighed against potential side effects, including increased intraocular pressure (which can lead to glaucoma) and cataract formation.
Managing Diabetes for Eye Health
Effective management of systemic diabetes is fundamental to preventing and controlling diabetic retinopathy. Tight glycemic control, blood pressure management, and cholesterol regulation are critical factors in reducing the risk of onset and progression of diabetic eye disease. Patients are strongly advised to:
- Maintain strict blood sugar control: Regular monitoring of blood glucose levels and adherence to prescribed insulin or oral medications are essential.
- Control blood pressure: High blood pressure exacerbates retinal damage, so maintaining it within healthy ranges is vital.
- Manage cholesterol levels: Elevated cholesterol can contribute to the formation of hard exudates and further compromise retinal health.
- Adopt a healthy lifestyle: A balanced diet, regular exercise, and smoking cessation significantly reduce systemic and ocular complications of diabetes.
- Attend regular eye examinations: Consistent monitoring by an ophthalmologist allows for early detection and prompt intervention, safeguarding vision.
Choosing Your Treatment Provider: Turkey vs. United Kingdom
International patients, particularly those from the United Kingdom, often explore options abroad for specialized medical care, including specialised eye treatments in Turkey. Turkey has emerged as a prominent destination for medical tourism, offering advanced healthcare facilities, experienced specialists, and competitive pricing without compromising on quality.
When considering diabetic retinopathy treatment, patients typically weigh factors such as cost, accessibility, technology, and specialist expertise. While the UK boasts a robust healthcare system through the NHS and private providers, waiting lists, and sometimes higher costs for specific private treatments can be a concern for some individuals. Turkey presents an attractive alternative, often providing immediate access to consultations and procedures, state-of-the-art equipment, and internationally trained ophthalmologists.
Price Comparison: Diabetic Retinopathy Treatment Costs
Navigating the financial aspects of medical treatment is crucial. Below is a comparative overview of estimated costs for common diabetic retinopathy treatment procedures in Turkey versus the United Kingdom. Prices are indicative and can vary based on the clinic, specific procedure, and individual patient needs. (All prices in GBP).
| Service/Item | Turkey Price (GBP) | United Kingdom Price (GBP) |
|---|---|---|
| Anti-VEGF Injection (per injection) | £300 – £600 | £800 – £1,500 |
| Retinal Laser Treatment (PRP) | £1,200 – £2,500 | £2,500 – £5,000 |
| Vitrectomy (uncomplicated) | £4,000 – £7,000 | £8,000 – £15,000 |
| OCT Scan (diagnostic) | £80 – £150 | £150 – £300 |
| Fluorescein Angiography | £150 – £300 | £300 – £600 |
Comparison of Treatment Modalities for Diabetic Macular Edema (DME)
| Factor | Anti-VEGF Injections | Laser Photocoagulation | Corticosteroid Injections |
|---|---|---|---|
| Mechanism | Blocks VEGF, reducing vessel growth & leakage | Seals leaking vessels, destroys ischemic tissue | Reduces inflammation & leakage |
| Efficacy for Vision Improvement | High, often improves visual acuity | Primarily stabilizes, less common for significant improvement | Moderate, can improve vision, good for refractory DME |
| Frequency of Treatment | Monthly initially, then tapered | Usually 1-3 sessions per eye | Less frequent, but can have side effects |
| Side Effects | Low risk of endophthalmitis, temporary floaters | Mild discomfort, possible peripheral vision loss | Increased intraocular pressure, cataract |
| Cost Consideration | Ongoing cost due to multiple injections | Single procedure cost, but may need repeat | Less frequent, but higher individual dose cost |
CK Health Turkey: Your Partner in Eye Health
For international patients considering medical care abroad, CK Health Turkey stands as a beacon of excellence, particularly for those seeking advanced eye treatments. We pride ourselves on offering world-class medical services, including comprehensive diagnostics and state-of-the-art diabetic retinopathy treatment options. Our facilities are equipped with the latest technology, and our team comprises highly skilled, board-certified ophthalmologists with extensive experience in managing complex diabetic eye conditions. We understand the unique needs of international patients, providing seamless coordination for travel, accommodation, and all aspects of your medical journey. Our commitment is to deliver not only superior clinical outcomes but also an empathetic and supportive experience, ensuring your comfort and peace of mind throughout your treatment process. For more information or to schedule a consultation, please visit our website or get in touch with our dedicated patient coordination team.
FAQs
What is diabetic retinopathy?
Diabetic retinopathy is an eye condition that can cause vision loss and blindness in people who have diabetes. It affects the blood vessels in the retina, the light-sensitive tissue at the back of the eye.
Who is at risk of developing diabetic retinopathy?
Anyone with type 1 or type 2 diabetes is at risk. The longer you have diabetes and the less controlled your blood sugar, the higher your risk. High blood pressure and high cholesterol also increase risk.
How is diabetic retinopathy detected?
It’s detected through a comprehensive dilated eye exam, which allows an ophthalmologist to examine the retina. Additional tests like fluorescein angiography and optical coherence tomography (OCT) may be used for detailed assessment.
What are the main treatment options for diabetic retinopathy?
The primary treatments include anti-VEGF injections, retinal laser treatment (photocoagulation), and vitrectomy for advanced cases. Corticosteroid injections are also an option for some patients with macular edema.
Are anti-VEGF injections painful?
The procedure involves a fine needle, but the eye is numbed with anesthetic eye drops, so most patients experience only mild pressure or discomfort. The injection itself is typically quick.
Can diabetic retinopathy be cured?
While it cannot be cured, its progression can be effectively managed and vision loss prevented or minimized with timely and appropriate treatment. Consistent diabetes management is key to long-term success.
How often do I need eye exams if I have diabetes?
Generally, annual dilated eye exams are recommended. However, your ophthalmologist may advise more frequent checks depending on the stage of your retinopathy and overall diabetes control.
What is the recovery time after a vitrectomy?
Recovery after vitrectomy varies, but initial healing typically takes a few weeks. Full visual recovery can take several months. Patients may need to maintain specific head positions and use eye drops as directed.
Can I travel for diabetic retinopathy treatment in Turkey if I’m from the UK?
Yes, many UK patients choose Turkey for eye treatments due to advanced facilities, experienced specialists, and competitive pricing. CK Health Turkey assists with all aspects of medical travel. You can also explore strategies for managing dry eye during and after treatment.
What role does diet play in managing diabetic retinopathy?
A healthy, balanced diet that helps manage blood sugar, blood pressure, and cholesterol levels is crucial. It supports overall diabetes control, which directly impacts the health of your eyes and the effectiveness of diabetic retinopathy treatment.