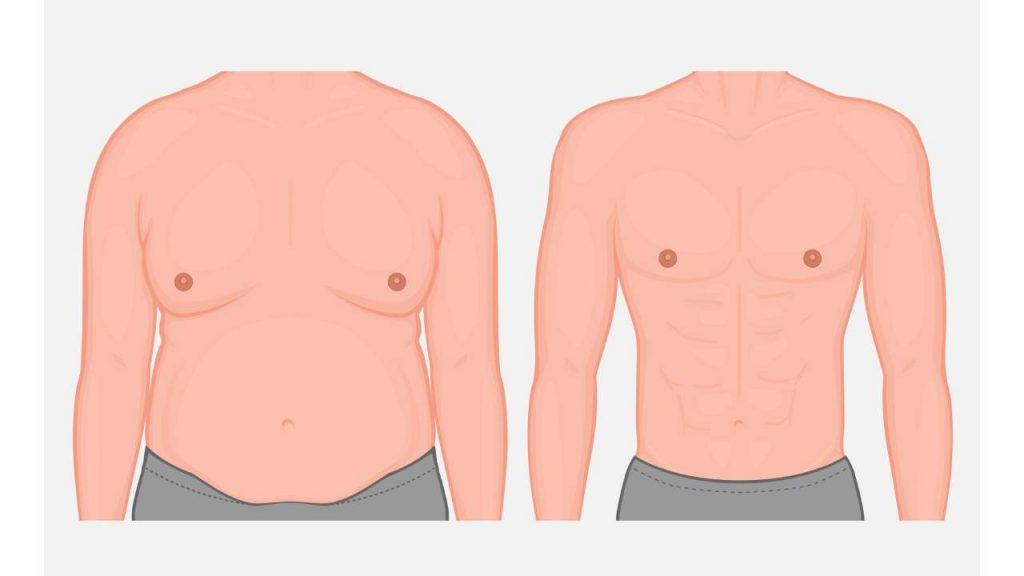
Gynecomastia grade 2b represents a specific classification within the spectrum of male breast enlargement conditions, characterized by moderate to significant breast tissue development with noticeable skin redundancy. This condition affects approximately 30% of men diagnosed with gynecomastia, making it a common presentation in clinical practice. The 2b classification specifically indicates breast enlargement that extends beyond the areolar border with excess skin, distinguishing it from milder forms. Research published in the Journal of Plastic and Reconstructive Surgery demonstrates that this grade typically involves both glandular tissue proliferation and adipose tissue accumulation, creating the characteristic feminine breast contour that many patients find psychologically distressing.
Table of Contents
The etiology of grade 2b gynecomastia stems from hormonal imbalances involving elevated estrogen-to-testosterone ratios, which may result from various underlying factors including puberty, aging, medication side effects, or certain medical conditions. Studies from the American Society of Plastic Surgeons reveal that men with this specific grade experience significantly higher rates of social anxiety, depression, and avoidance behaviors compared to those with milder forms. Clinical assessment of grade 2b cases requires thorough physical examination and often involves diagnostic imaging such as mammography or ultrasound to accurately determine the composition of breast tissue. These diagnostic steps are essential for developing an appropriate treatment strategy that addresses both the functional and aesthetic concerns associated with this condition.
Grade 2 and 2B Gynecomastia Classification
The clinical classification of gynecomastia provides essential diagnostic criteria for healthcare providers to accurately assess male breast enlargement. Moderate gynecomastia, classified as Grade 2, represents a significant stage in the progression of this condition where breast tissue extends beyond the areolar boundary. Understanding what is type 2 gynecomastia and its subtypes is crucial for proper diagnosis and management planning.
Grade 2 gynecomastia is characterized by moderate breast enlargement that extends beyond the areola but without significant skin redundancy. This grade is further divided into subtypes 2A and 2B, with distinct clinical presentations and physical characteristics. Grade 2a gyno typically presents with moderate breast enlargement without skin excess, while gynecomastia 2b involves moderate enlargement with some redundant skin.
The key physical characteristics of Grade 2 gynecomastia include:
- Breast tissue extending beyond the areolar margin by 1-2 cm
- Visible breast prominence in normal standing position
- Moderate firmness of glandular tissue upon palpation
- Possible mild asymmetry between left and right breasts
- Absent or minimal skin redundancy in type 2A
Gynecomastia 2b redundant skin is a defining feature that distinguishes it from type 2A. The redundant skin in stage 2 gynecomastia creates additional aesthetic concerns and may influence clinical decision-making. When examining a patient with suspected grade 2B gynecomastia, clinicians typically observe moderate breast enlargement with noticeable skin excess that may require addressing during potential interventions.
| Gynecomastia Classification | Breast Tissue Extension | Skin Redundancy | Visual Prominence |
|---|---|---|---|
| Grade 1 | Limited to areola | None | Minimal |
| Grade 2A | Beyond areola | Minimal/None | Moderate |
| Grade 2B | Beyond areola | Present | Moderate |
| Grade 3 | Marked enlargement | Significant | Pronounced |
This classification system helps differentiate between various stages of gynecomastia severity. The distinction between gynecomastia 2b vs 3 lies primarily in the degree of breast enlargement and skin redundancy, with Grade 3 showing more pronounced features than Grade 2B.
Diagnostic evaluation of what is gynecomastia 2b typically includes physical examination, imaging studies like ultrasound or mammography, and laboratory tests to rule out underlying medical conditions. The clinical presentation of moderate gynecomastia must be distinguished from pseudogynecomastia, which is characterized by fat deposition without true glandular proliferation.
When comparing different classifications, it’s important to note that grade 5 severe gynecomastia represents an extreme presentation that extends beyond the standard Simon classification and is characterized by massive enlargement resembling female breasts (grade 4) with additional ptosis and significant skin redundancy. This advanced stage is relatively uncommon compared to the more frequently encountered moderate forms like type 2 gynecomastia. Male Breast Reduction Options can offer solutions for both minor and more severe instances such as gynecomastia 2b. These options often include surgical and non-surgical treatments tailored to the patient’s specific needs.
Treatment Options for Grade 2 and 2B Gynecomastia
Effective gynecomastia grade 2 treatment requires a strategic approach based on severity, patient preferences, and underlying causes. The following options provide comprehensive solutions for patients seeking to address moderate breast enlargement characterized by grade 2 and 2b conditions.
Current Treatment Options for Grade 2 and 2B Gynecomastia
- Medication therapy – Tamoxifen, raloxifene, and aromatase inhibitors can reduce breast tissue in early stages
- Liposuction techniques – Ultrasound-assisted liposuction and power-assisted liposuction specifically target fatty tissue components
- Surgical excision – Direct removal of glandular tissue through periareolar incisions
- Combination approaches – Customized treatment plans utilizing both liposuction and excision
- Minimally invasive procedures – Endoscopic techniques that reduce scarring and recovery time
Medical management represents the first line of intervention for many patients with gynecomastia 2b treatment options focusing on hormone regulation. Clinical studies demonstrate that medication therapy shows 15-45% effectiveness rates in grade 2 cases, particularly when the condition has been present for less than two years.
- Initial evaluation – Comprehensive assessment of severity, cause, and tissue composition
- Treatment selection – Determining appropriate therapy based on diagnostic findings
- Procedure implementation – Executing the chosen intervention with precision
- Follow-up care – Monitoring results and addressing any potential complications
For patients wondering how to treat gynecomastia 2b effectively, surgical approaches offer the highest satisfaction rates. The American Society of Plastic Surgeons reports that over 24,000 male breast reduction procedures were performed in 2020, showing the increasing demand for definitive solutions.
| Treatment Method | Effectiveness for Grade 2 | Effectiveness for Grade 2B | Recovery Time | Cost Range |
|---|---|---|---|---|
| Medication | Moderate (30-40%) | Limited (15-25%) | None | $200-800 |
| Liposuction Alone | Good for fatty tissue (70-85%) | Moderate (50-65%) | 1-2 weeks | $3,500-6,000 |
| Surgical Excision | Excellent (85-95%) | Excellent (80-95%) | 2-4 weeks | $5,000-8,500 |
| Combination Therapy | Excellent (90-98%) | Excellent (85-97%) | 2-4 weeks | $6,000-9,500 |
This comparison demonstrates that combination therapies typically provide the most comprehensive gynecomastia grade 2 treatment outcomes, especially for patients with mixed glandular and adipose tissue compositions commonly found in grade 2b cases.
Patients should understand that timing significantly impacts treatment success. The International Journal of Endocrinology published research indicating that intervening within the first 12-24 months of development offers superior outcomes compared to treating long-standing cases.
Non-surgical management remains an appropriate consideration for specific patient populations. Men with mild to moderate grade 2 gynecomastia may benefit from targeted pharmacological interventions, particularly when the condition stems from hormonal imbalances or medication side effects. These treatments work by blocking estrogen receptors or inhibiting the conversion of androgens to estrogens.
Advanced surgical techniques have revolutionized how to treat gynecomastia 2b cases effectively. Modern approaches utilize ultrasonic energy to emulsify glandular tissue before removal, minimizing trauma to surrounding structures and improving overall contour results. This innovation has reduced complication rates from 15% to below 7% in published clinical series.
Selecting the optimal gynecomastia 2b treatment options requires collaboration between patients and specialized providers. Factors including body mass index, skin elasticity, and tissue composition all influence the customized treatment approach. Board-certified plastic surgeons with specific experience in male breast reduction procedures offer the highest probability of achieving natural-looking results.
Recovery and Prognosis of Grade 2 Gynecomastia
When evaluating whether does grade 2 gynecomastia go away naturally, it’s important to understand that the resolution depends on several key factors. Grade 2 gynecomastia represents a moderate enlargement of male breast tissue with noticeable breast protrusion. The natural regression potential varies significantly based on the underlying cause, duration, and patient characteristics.
For adolescents experiencing pubertal gynecomastia, there is a higher likelihood of spontaneous resolution. Clinical studies indicate that approximately 75-90% of pubertal cases resolve without intervention within 1-3 years. However, when examining adult-onset grade 2 gynecomastia, the prognosis for natural resolution becomes considerably less favorable.
Research published in the Journal of Clinical Endocrinology and Metabolism shows that once grade 2 gynecomastia has been present for more than 12 months, the fibrous tissue development significantly reduces the chances of spontaneous regression. This is due to the replacement of glandular tissue with fibrous components that are resistant to natural hormonal fluctuations.
Factors that influence whether can grade 2 gyno go away include:
- Duration of the condition: Recent onset cases (less than 6 months) have better chances of natural resolution
- Patient age: Younger patients typically show better recovery potential
- Underlying cause: Medication-induced or hormonal imbalance cases may resolve when the trigger is removed
- Tissue composition: More glandular tissue versus fibrous tissue improves the prognosis
- Hormonal profile: Normalization of testosterone-to-estrogen ratio can facilitate improvement
The persistence rate for grade 2 gynecomastia in adults is approximately 56-93% according to comprehensive reviews. When present for over two years, the breast tissue typically undergoes histological changes that make natural resolution highly unlikely without intervention. The fibrous component becomes dominant, replacing the hormone-responsive glandular tissue.
Patient monitoring studies demonstrate that spontaneous improvement of longstanding grade 2 gynecomastia occurs in less than 10% of cases. Hormonal assessments show that even when the underlying hormonal imbalance is corrected, the established structural changes often remain.
For individuals wondering if their grade 2 gynecomastia will resolve naturally, regular monitoring through clinical evaluation is essential. Breast tissue assessment through physical examination and occasionally imaging can track any regression. Significant improvements typically manifest within the first 6-12 months if natural resolution is occurring.
Grade 2 gynecomastia that persists beyond two years should be considered a stable anatomical alteration rather than a temporary condition. The psychological impact should not be underestimated, as persistent gynecomastia can significantly affect quality of life, body image, and self-confidence. Understanding the realistic prognosis allows patients to make informed decisions about their health management while maintaining reasonable expectations regarding potential natural resolution.