Gastric bypass surgery profoundly alters the digestive system, aiming for significant and lasting weight loss. While highly effective for many, a subset of patients may experience complications or inadequate outcomes over time. These issues, ranging from severe nutritional deficiencies to persistent chronic pain or weight regain, necessitate careful consideration. Clinical data indicates that up to 10% of patients may require further intervention due to these challenges. Reversal of gastric bypass surgery emerges as a complex, highly specialized procedure. This intervention is reserved for specific, compelling medical indications. It demands a thorough understanding of patient physiology and surgical principles. The decision to reverse a gastric bypass involves comprehensive patient evaluation and risk assessment.
Table of Contents
Which Weight Loss Surgeries Can Be Reversed and How?
Gastric band procedures demonstrate the highest reversibility rates among bariatric surgeries, with surgeons typically removing the adjustable silicone band through minimally invasive techniques. The gastric band reversal process involves deflating the band and surgically extracting it, allowing the stomach to return to its original configuration. Clinical studies indicate that approximately 95% of patients experience complete anatomical restoration following band removal.
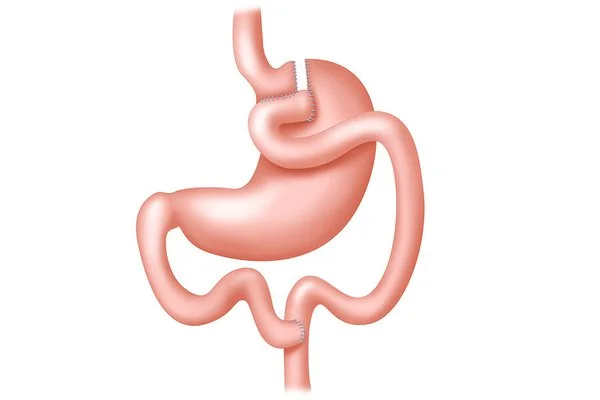
Gastric bypass reversal feasibility varies significantly based on the surgical technique initially employed. Roux-en-Y gastric bypass reversals require complex reconstruction of the digestive tract, reconnecting the bypassed stomach portion and restoring normal intestinal anatomy. Reversal success rates range between 75-85% for experienced bariatric teams, though the procedure carries substantially higher risks than the original surgery.
The question “is gastric bypass reversible” generates considerable patient interest, particularly when complications arise. Surgeons evaluate multiple factors including patient health status, original surgical technique, and anatomical changes before determining candidacy. Complete reversal remains technically challenging due to extensive anatomical modifications made during the initial procedure.
Gastric sleeve surgery reversal presents unique complexities since the procedure permanently removes approximately 80% of the stomach. Can bariatric surgery be reversed in sleeve gastrectomy cases? Traditional reversal proves impossible due to tissue removal, though surgeons occasionally perform conversions to alternative procedures like gastric bypass to address complications.
Reverse gastric bypass reversal procedures require sophisticated surgical expertise and comprehensive preoperative evaluation. Patients considering reversal typically undergo extensive metabolic assessments, nutritional evaluations, and psychological consultations. Conversion surgeries offer alternative solutions when complete reversal proves unfeasible, allowing surgeons to modify existing anatomy while maintaining some weight management benefits. Success depends heavily on individual anatomical factors, surgical history, and specific medical circumstances surrounding the reversal request. Gastric Bypass Complications can significantly influence the decision-making process for gastric bypass surgery reversal. These complexities necessitate a tailored approach to ensure optimal outcomes for each patient.
What Makes Gastric Bypass Reversal Necessary?
Several serious medical complications and adverse outcomes can make gastric bypass reversal essential for patient health and quality of life. Understanding these reasons helps patients and healthcare providers recognise when this complex procedure becomes medically warranted.
Excessive weight loss represents one of the most concerning complications requiring intervention. When patients lose significantly more weight than intended, reaching dangerously low body mass indices, malnutrition and organ dysfunction can occur. This gastric bypass reversal excessive weight loss scenario often develops months or years post-surgery, affecting the body’s ability to maintain essential functions.
Chronic complications from the original procedure constitute another major category of reasons for gastric bypass reversal:
- Persistent marginal ulceration at the gastrojejunal anastomosis that fails to heal despite medical management
- Severe dumping syndrome causing debilitating symptoms including rapid heart rate, sweating, and gastrointestinal distress
- Chronic malabsorption syndromes leading to deficiencies in essential vitamins, minerals, and nutrients
- Anastomotic strictures causing recurrent food blockages and eating difficulties
Gastric bypass reversal chronic pain frequently stems from adhesions, bowel obstructions, or nerve entrapment following the initial surgery. This persistent discomfort significantly impacts daily functioning and requires comprehensive evaluation to determine if anatomical restoration would provide relief.
Psychological and social factors also contribute to reasons to reverse gastric bypass. Some patients experience severe eating disorders, inability to maintain proper nutrition, or profound regret about their decision. These psychological complications often intertwine with physical symptoms, creating complex clinical scenarios.
Pregnancy-related complications present unique circumstances where reversing gastric bypass complications becomes necessary. Severe malnutrition during pregnancy can threaten both maternal and foetal health, making reversal a potentially life-saving intervention.
Medication absorption issues pose another significant concern. Patients requiring specific medications for chronic conditions may experience therapeutic failures due to altered gastrointestinal anatomy, necessitating surgical correction to restore normal drug absorption patterns.
Each case requires thorough evaluation by experienced bariatric surgeons who can assess the risk-benefit ratio of reversal versus alternative management strategies.
Understanding the Gastric Bypass Reversal Process
The gastric bypass reversal procedure represents a complex surgical intervention that restores the original digestive anatomy following previous bariatric surgery. Our surgical experience demonstrates that understanding the comprehensive reversal process requires detailed knowledge of multiple restoration techniques and anatomical considerations.
Roux-en-Y Reversal Techniques
Roux-en-Y gastric bypass reversal involves specialized surgical protocols that systematically address the modified digestive structures created during the initial bariatric procedure.
- Gastrojejunostomy disconnection forms the initial step, where surgeons carefully separate the stomach pouch from the jejunal limb while preserving surrounding tissue integrity and vascular supply.
- Stomach reconstruction follows through meticulous suturing techniques that restore the original gastric capacity, requiring precise tissue alignment to ensure proper healing and functionality.
- Jejunal restoration involves reconnecting the proximal jejunum to the duodenum, re-establishing the natural flow of digestive enzymes and bile acids through the alimentary tract.
- Anastomotic revision completes the technical sequence by creating secure connections between restored anatomical structures using advanced suturing materials and reinforcement techniques.
Alternative Surgical Approaches
Various surgical options for gastric bypass reversal accommodate different patient anatomies and clinical presentations beyond standard reversal protocols.
- Laparoscopic reversal techniques utilise minimally invasive approaches with five-port configurations for reduced tissue trauma and enhanced visualisation of anatomical structures
- Open surgical methods provide comprehensive access for complex cases involving significant adhesions or anatomical variations requiring extensive reconstruction
- Hybrid approaches combine laparoscopic and open techniques based on intraoperative findings and individual patient requirements
- Staged reversal procedures address complex cases through multiple surgical sessions, allowing optimal healing between reconstruction phases
Step-by-Step Restoration of Digestive Anatomy
The bariatric surgery gastric bypass reversal process systematically rebuilds normal digestive function through sequential anatomical restoration that addresses each modified structure.
- Peritoneal cavity assessment begins the restoration process through comprehensive evaluation of adhesions, anatomical changes, and tissue viability throughout the surgical field.
- Gastric pouch mobilisation involves careful dissection of the small stomach pouch from surrounding structures while maintaining adequate blood supply for subsequent reconstruction procedures.
- Duodenal identification requires precise localisation of the original duodenal anatomy, often complicated by scarring and adhesion formation from previous surgical interventions and healing processes.
- Anatomical reconstruction completes the reversal through systematic reconnection of stomach, duodenum, and jejunum using tension-free anastomotic techniques that ensure long-term structural integrity and optimal digestive function.
Safety and Recovery: What to Expect After Reversal
Gastric bypass reversal safety represents a significant concern for patients considering this complex procedure. The operation carries inherent risks, with mortality rates ranging from 1-3% according to current surgical data. Gastric bypass reversal complications include anastomotic leaks, bleeding, infection, and bowel obstruction, requiring careful postoperative monitoring by experienced surgical teams.
The most frequently encountered gastric bypass reversal side effects during the initial recovery phase include:
- Severe abdominal pain requiring prescription pain management
- Nausea and vomiting lasting several days post-surgery
- Temporary difficulty maintaining adequate nutritional intake
- Fatigue and weakness due to metabolic adjustments
- Potential dumping syndrome as digestive patterns readjust
Gastric bypass reversal recovery time varies significantly between patients, typically extending 8-12 weeks for complete healing. The first two weeks demand strict dietary restrictions, progressing from clear liquids to soft foods under medical supervision. Most patients resume normal activities within 4-6 weeks, though full recovery depends on individual healing capacity and adherence to postoperative protocols.
Long-term safety considerations encompass nutritional deficiencies, weight regain patterns, and gastrointestinal function restoration. Patients frequently experience gastric bypass reversal experience challenges including altered appetite regulation and digestive sensitivity. Regular follow-up appointments monitor liver function, vitamin levels, and overall metabolic health during the extended recovery period.
Recovery milestones typically follow this progression:
- Hospital discharge within 2-4 days post-surgery
- Return to light activities after 2-3 weeks
- Full dietary progression completed by week 6-8
- Complete wound healing achieved within 8-10 weeks
- Metabolic stabilisation occurring over 3-6 months
Successful outcomes depend heavily on patient compliance with dietary modifications, vitamin supplementation, and regular medical monitoring. Surgeons emphasise that reversal procedures demand greater technical complexity than original bypass surgery, necessitating specialised expertise and comprehensive preoperative evaluation. The procedure’s success relies on meticulous surgical technique, appropriate patient selection, and dedicated postoperative care protocols to minimise complications and optimise recovery outcomes.