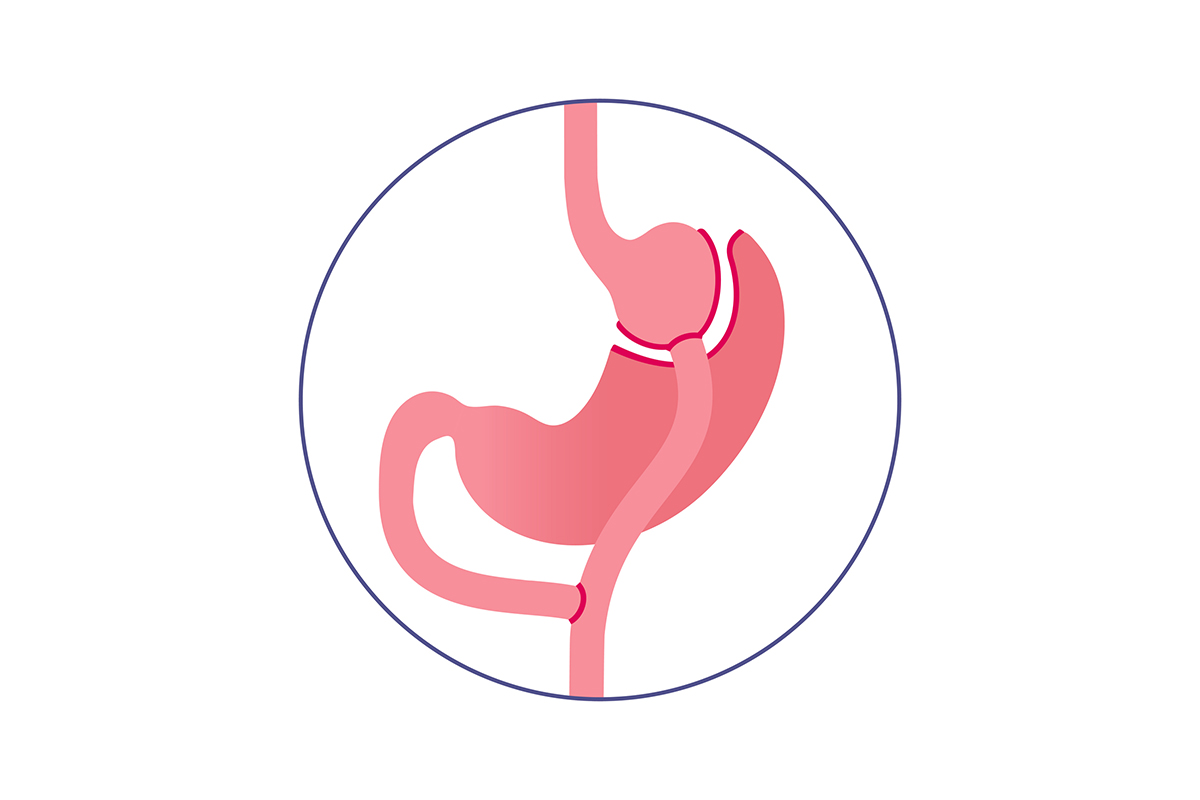
Mini gastric bypass surgery, a streamlined alternative to traditional gastric bypass procedures, presents a specific profile of potential side effects that patients should understand before committing to the procedure. Clinical data from recent longitudinal studies demonstrates that while this procedure offers significant weight loss benefits, it comes with unique physiological challenges. The reduced surgical complexity compared to Roux-en-Y procedures doesn’t necessarily translate to reduced complications; rather, it shifts the risk profile toward different concerns including bile reflux, nutritional deficiencies, and marginal ulcers. Research published in the Journal of Bariatric Surgery shows that approximately 15-20% of patients experience some form of malnutrition, particularly deficiencies in vitamin B12, iron, and calcium within the first year post-operation.
Table of Contents
The metabolic changes resulting from mini bypass also create potential long-term challenges that extend beyond the immediate surgical recovery period. Patients frequently report dumping syndrome, characterized by nausea, vomiting, and abdominal discomfort after consuming high-sugar foods, affecting quality of life for 30-50% of recipients to varying degrees. Bone health complications emerge as another significant concern, with studies documenting a 15% reduction in bone mineral density among some patients within three years of surgery. These physiological responses occur due to the procedure’s alteration of nutrient absorption pathways and hormonal mechanisms that regulate hunger, satiety, and digestive processes. Understanding these complex biological responses helps patients develop realistic expectations about post-surgical adjustments and necessary lifestyle modifications.
Specific Bypass Surgery Types and Their Complications
Each bariatric surgery technique has unique physiological effects on the digestive system, leading to distinct potential complications. Understanding these specific risks is essential for patients considering various weight loss surgery options.
Roux-en-Y Gastric Bypass: Unique Complications
- Dumping syndrome: Rapid emptying of stomach contents into small intestine, affecting 15-20% of patients
- Anastomotic strictures: Narrowing at the connection between stomach pouch and small intestine
- Internal hernias: Intestinal loops slip through surgically created spaces in abdomen
- Marginal ulcers: Painful sores developing at the junction of stomach pouch and small intestine
- Nutritional deficiencies: Particularly vitamin B12, iron, calcium, and folate
- Bowel obstruction: Blockage preventing food or liquid from passing through intestines
| Complication | Severity | Incidence Rate |
|---|---|---|
| Dumping Syndrome | Mild to Moderate | 15-20% |
| Anastomotic Stricture | Moderate | 5-10% |
| Internal Hernias | Severe | 2-5% |
| Marginal Ulcers | Moderate | 5-15% |
| Nutritional Deficiencies | Mild to Severe | 30-50% |
| Bowel Obstruction | Severe | 1-3% |
Patients who undergo Roux-en-Y procedures typically require lifelong vitamin supplementation and regular blood tests to monitor nutritional status. The anatomical changes in this procedure create several points where complications can develop, though modern surgical techniques have reduced overall complication rates.
Mini Gastric Bypass: Unique Complications
- Bile reflux gastritis: Bile backing up into the stomach pouch causing inflammation
- Malabsorption issues: Reduced absorption of essential nutrients
- Marginal ulceration: Higher rates than with traditional gastric bypass
- Metabolic bone disease: Due to calcium and vitamin D malabsorption
- Protein-calorie malnutrition: Inadequate protein intake or absorption
- Dental problems: Related to frequent vomiting and nutritional deficiencies
| Complication | Severity | Incidence Rate |
|---|---|---|
| Bile Reflux | Moderate to Severe | 1-5% |
| Malabsorption | Moderate | 10-15% |
| Marginal Ulceration | Moderate | 5-15% |
| Metabolic Bone Disease | Moderate to Severe | 10-25% |
| Protein Malnutrition | Severe | 1-3% |
| Dental Issues | Mild to Moderate | 10-15% |
The disadvantages of mini gastric bypass include its single anastomosis design, which creates potential for bile reflux issues. This procedure’s simplicity offers surgical advantages, but one anastomosis gastric bypass side effects may be more pronounced in terms of nutritional complications compared to other techniques.
Biliopancreatic Diversion with Duodenal Switch: Unique Complications
- Severe malnutrition: Most pronounced among all bariatric procedures
- Protein deficiency: Can lead to muscle wasting and weakness
- Fat-soluble vitamin deficiencies: Vitamins A, D, E, and K
- Steatorrhea: Excess fat in stool due to malabsorption
- Diarrhea and frequent bowel movements: Common ongoing issue
- Kidney stones: Due to oxalate absorption changes
| Complication | Severity | Incidence Rate |
|---|---|---|
| Protein Deficiency | Severe | 12-18% |
| Fat-soluble Vitamin Deficiencies | Severe | 50-60% |
| Steatorrhea | Moderate | 40-50% |
| Diarrhea | Moderate to Severe | 30-50% |
| Kidney Stones | Moderate | 8-10% |
| Anemia | Moderate to Severe | 30-35% |
This procedure creates the most significant malabsorptive effect, resulting in excellent weight loss but requiring the most intensive nutritional monitoring and supplementation among all bariatric procedures.
Adjustable Gastric Banding: Unique Complications
- Band slippage: Stomach tissue slides through the band
- Band erosion: Band erodes into stomach tissue
- Port problems: Infection, displacement, or leakage of port system
- Esophageal dilation: Enlargement of esophagus above the band
- Pouch dilation: Enlargement of stomach pouch above the band
| Complication | Severity | Incidence Rate |
|---|---|---|
| Band Slippage | Moderate to Severe | 3-8% |
| Band Erosion | Severe | 1-3% |
| Port Problems | Mild to Moderate | 5-10% |
| Esophageal Dilation | Moderate | 5-8% |
| Pouch Dilation | Moderate | 10-15% |
While adjustable gastric banding offers reversibility, its unique hardware-related complications often necessitate reoperation, contributing to its declining popularity in recent years.
Sleeve Gastrectomy: Unique Complications
- Gastric leak: Potentially life-threatening leak along staple line
- Stenosis: Narrowing of the gastric sleeve
- GERD: New or worsened gastroesophageal reflux disease
- Vitamin B12 deficiency: Due to reduced intrinsic factor production
- Sleeve dilation: Gradual enlargement of the sleeve over time
| Complication | Severity | Incidence Rate |
|---|---|---|
| Gastric Leak | Severe | 1-3% |
| Stenosis | Moderate | 1-4% |
| GERD | Mild to Severe | 10-20% |
| Vitamin B12 Deficiency | Mild to Moderate | 10-15% |
| Sleeve Dilation | Moderate | 5-10% |
Gastric bypass sleeve side effects tend to focus more on mechanical and structural issues rather than severe malabsorptive complications. The mini gastric sleeve variation may offer reduced operative time but maintains similar complication profiles to traditional sleeve procedures. Gastric Bypass Eligibility is a key consideration for patients evaluating the potential benefits and risks associated with mini bypass side effects. Understanding the comprehensive impact on lifestyle and health outcomes can guide individuals in making informed decisions about their surgical options.
Mini Gastric Bypass Surgery Complications Timeline
Understanding the timeline of potential complications following mini gastric bypass surgery is crucial for patients considering this procedure. Awareness of when specific adverse effects might occur helps in early detection and proper management.
Immediate Post-Operative Complications
The first 48 hours after mini gastric bypass surgery present several potential complications that require vigilant monitoring:
- Anastomotic leakage at the surgical connection points
- Excessive bleeding from surgical sites
- Adverse reactions to anesthesia including nausea and respiratory issues
- Pulmonary embolism resulting from blood clots
- Wound infections at incision sites
- Patients must monitor for signs of fever, increasing pain, or unusual drainage from incisions
- Regular vital sign monitoring helps detect mini gastric bypass complications early
- Following strict post-surgery protocols reduces the risk of immediate complications
- Proper hydration within medical guidelines supports initial healing
Early Post-Operative Complications (First Weeks)
During the first few weeks following surgery, patients may experience various mini bypass side effects as the body adjusts to the anatomical changes:
- Dumping syndrome characterized by nausea, vomiting, and diarrhea after eating
- Nutritional deficiencies beginning to manifest
- Dehydration due to reduced fluid intake
- Nausea and vomiting from dietary transitions
- Temporary hair loss related to nutritional changes and surgical stress
- Adhering to the prescribed post-operative diet minimizes early complications
- Regular follow-up appointments allow for monitoring of healing progress
- Supplementation with prescribed vitamins helps prevent early deficiencies
- Gradual introduction of foods reduces the risk of gastric bypass recovery problems
Late Complications and Long-Term Risks
Long-term mini bypass adverse effects may develop months or even years after the procedure, requiring ongoing vigilance:
- Malnutrition particularly deficiencies in iron, calcium, and vitamins B12 and D
- Marginal ulcers at the connection between the stomach pouch and intestine
- Intestinal obstruction from adhesions or internal herniation
- Bile reflux gastritis causing persistent discomfort
- Weight regain after initial success
- Hypoglycemia particularly after consuming carbohydrates
| Long-term Mini Bypass Complications | Estimated Prevalence | Typical Onset |
|---|---|---|
| Nutritional deficiencies | 30-50% | 6+ months |
| Marginal ulcers | 5-15% | 3+ months |
| Bile reflux | 10-20% | 1+ years |
| Internal hernias | 1-5% | 1-3 years |
| Weight regain | 15-25% | 2+ years |
The data shows that nutritional deficiencies represent the most common long-term side effects of mini gastric bypass, affecting up to half of all patients. While some complications like marginal ulcers tend to appear within months of surgery, others such as internal hernias may not manifest until years later. This emphasizes the importance of lifelong monitoring following the procedure to identify potential mini bypass long-term side effects before they become severe health risks.
Treatment and Management of Bypass Surgery Complications
The comprehensive management of gastric bypass complications requires a multidisciplinary approach involving surgeons, gastroenterologists, dietitians, and other specialists. Effective treatment strategies must address both immediate and long-term issues that patients may experience following their procedure. Bariatric surgery side effectsrange from minor discomforts to potentially life-threatening conditions that require prompt intervention.
General Management Principles for Bypass Complications
- Early recognition is crucial in managing complications from weight loss surgery, with regular follow-up appointments helping to identify issues before they become severe
- Nutritional monitoring addresses deficiencies that often occur following gastric bypass surgery
- Medication adjustments may be necessary as absorption patterns change after surgery
- Hydration maintenance is essential for preventing complications related to dehydration
- Psychological support helps patients cope with unexpected outcomes and adherence challenges
- Radiological imaging assists in diagnosing structural complications that may develop over time
The multidisciplinary team approach ensures that all aspects of gastric bypass dangerous side effects are addressed promptly and effectively. Treatment plans must be tailored to each patient’s specific condition, medical history, and surgical outcome.
Acute Complications Management
Immediate intervention is often required for acute complications that develop shortly after surgery. These complications can be life-threatening if not treated promptly.
- Hemorrhage management begins with hemodynamic stabilization, fluid resuscitation, and blood transfusions if necessary
- Anastomotic leak treatment typically requires surgical intervention, drainage of collections, and aggressive antibiotic therapy
- Bowel obstruction resolution may involve nasogastric decompression and possible surgical correction
- Pulmonary embolism therapy includes anticoagulation, oxygen supplementation, and respiratory support
- Wound infection control requires appropriate antibiotics, regular dressing changes, and potential surgical debridement
Research indicates that approximately 5-10% of patients experience acute bariatric surgery complications requiring medical attention within the first 30 days post-surgery. Early intervention dramatically improves outcomes and reduces the risk of progression to chronic issues.
Chronic Complications Management
Long-term gastric bypass chronic complications require ongoing monitoring and treatment strategies. These conditions may develop months or years after the initial procedure and can significantly impact quality of life.
- Nutritional deficiency correction involves supplementation with vitamins (B12, D, A, K), minerals (iron, calcium), and protein
- Dumping syndrome management focuses on dietary modifications, medication therapy, and possible surgical revision in severe cases
- Marginal ulcer treatment includes proton pump inhibitors, elimination of NSAIDs, smoking cessation, and potential endoscopic or surgical intervention
- Stricture or stenosis therapy typically begins with endoscopic balloon dilation and may progress to surgical revision if unsuccessful
- Chronic abdominal pain assessment requires thorough diagnostic evaluation to identify the specific cause before appropriate treatment
- Internal hernia correction necessitates surgical intervention to prevent bowel ischemia and necrosis
Studies show that up to 30% of patients may experience some form of chronic complication following gastric bypass surgery. Regular nutritional assessments are particularly important, as nutrient deficiencies affect more than 50% of patients within five years of surgery if not properly supplemented.
Revisional Surgery Considerations
When conservative management fails to address severe weight loss surgery complications, revisional surgery may become necessary. This decision requires careful evaluation of risks versus benefits, especially considering that revisional procedures typically carry higher complication rates than primary surgeries.
The management of bariatric surgery complications has evolved significantly over the past decade, with improved surgical techniques, enhanced nutritional protocols, and better patient education contributing to better outcomes. Proactive monitoring remains the cornerstone of complication prevention and treatment, allowing for earlier intervention before complications become severe. Patients experiencing any unusual symptoms following gastric bypass should consult their surgical team immediately, as early treatment of complications significantly improves prognosis and reduces the likelihood of permanent damage.