Gastric bypass surgery represents a significant advancement in bariatric medicine, offering a scientifically proven approach to sustainable weight loss for individuals suffering from severe obesity. This surgical procedure fundamentally alters the digestive system by creating a smaller stomach pouch and rerouting the small intestine, effectively restricting food intake and reducing nutrient absorption. Clinical studies consistently demonstrate that patients lose 60-80% of their excess weight within the first year post-surgery, with many maintaining substantial weight loss long-term. The primary purpose extends beyond mere aesthetic improvements, as gastric bypass surgery addresses obesity-related comorbidities that significantly impact quality of life and mortality rates.
Table of Contents
The therapeutic benefits of gastric bypass surgery encompass substantial improvements in type 2 diabetes, often resulting in complete remission within days of the procedure—even before significant weight loss occurs. Research published in the New England Journal of Medicine confirms that 83% of patients experience resolution of diabetes following gastric bypass. Additionally, the procedure effectively reduces hypertension in 75% of patients, improves sleep apnea in 86% of cases, and alleviates joint pain associated with excess weight. These metabolic improvements occur through complex hormonal changes that regulate hunger, satiety, and glucose metabolism. Patients typically report enhanced mobility, reduced medication requirements, and improved psychological well-being, demonstrating the comprehensive health benefits this surgical intervention provides.
Types and Variations of Weight Loss Surgery
Bariatric surgery encompasses several distinct procedures, each with specific technical approaches and anatomical modifications. The choice between gastric bypass vs gastric sleeve or other weight loss surgery types depends on individual patient factors and surgical considerations.
Gastric Bypass Surgery
- Roux-en-Y gastric bypass represents the most common type of gastric bypass procedure performed worldwide
- Mini-gastric bypass features a single anastomosis technique with simplified surgical steps
- Distal gastric bypass involves a longer intestinal bypass component for enhanced malabsorption
- Banded gastric bypass incorporates a restrictive band around the pouch to enhance long-term results
- Fobi pouch gastric bypass utilizes a silastic ring to prevent pouch dilation over time
Sleeve Gastrectomy
- Standard sleeve gastrectomy removes approximately 80% of the stomach along the greater curvature
- Calibrated sleeve gastrectomy utilizes bougie sizes from 32-40Fr to standardize pouch creation
- Modified sleeve gastrectomy preserves the antrum to maintain physiological gastric emptying
- Robotic sleeve gastrectomy leverages advanced technology for enhanced surgical precision
Adjustable Gastric Banding
- LAGB (Laparoscopic Adjustable Gastric Banding) places an inflatable silicone device around the upper stomach
- AP Band features a low-pressure system with improved comfort and reduced complications
- Vertical banded gastroplasty combines stomach stapling with a band reinforcement
- Gastric balloon provides temporary restriction through an intragastric inflatable device
Biliopancreatic Diversion with Duodenal Switch
- Classic duodenal switch preserves the pyloric valve while creating significant malabsorption
- Two-stage BPD/DS separates the sleeve and intestinal components into sequential procedures
- Laparoscopic BPD/DS offers minimally invasive benefits for this complex procedure
- Single-anastomosis modification simplifies the traditional technique while maintaining efficacy
Single-Anastomosis Duodeno-Ileal Bypass with Sleeve Gastrectomy (SADI-S)
- Standard SADI-S combines vertical sleeve gastrectomy with a single-anastomosis duodeno-ileal bypass
- Modified SADI-S adjusts common channel length based on patient BMI and metabolic parameters
- Loop duodenal switch represents a technical variation with altered anatomical connections
- SIPS (Stomach Intestinal Pylorus Sparing) procedure preserves more natural digestive functionality
- Robotic SADI-S employs computer-assisted precision for enhanced technical execution
Goals and Benefits of Gastric Bypass Surgery
The purpose of gastric bypass surgery extends far beyond mere weight reduction, offering comprehensive health improvements for patients struggling with severe obesity. The primary benefits and objectives of this transformative bariatric procedure include:
- Significant weight loss is the fundamental goal of gastric bypass, with patients typically losing 60-80% of excess body weight within the first year after surgery.
- Resolution or improvement of obesity-related health conditions including type 2 diabetes, often occurring within days after Roux-en-Y gastric bypass, even before substantial weight loss.
- Reduction in cardiovascular risk factors such as hypertension, high cholesterol, and sleep apnea, which dramatically decreases heart disease risk.
- Enhanced quality of life through improved mobility, reduced joint pain, and increased energy levels, allowing patients to engage more fully in daily activities.
- Long-term maintenance of weight loss is achieved through the combined restrictive and malabsorptive mechanisms of stomach reduction procedures.
- Psychological benefits including improved self-esteem, reduced depression, and better social functioning as weight loss goals are achieved.
- Decreased medication dependency for conditions like hypertension and diabetes, providing both health and economic benefits.
- Prolonged life expectancy with studies showing that the weight loss surgery objectives, when met, can add years to a patient’s life through reduced comorbidities.
Eligibility and Requirements for Surgery
Gastric bypass surgery candidates must meet specific medical criteria established by healthcare professionals to ensure safe outcomes and maximize benefits. Patients seeking this intervention for severe weight issues should understand these requirements before proceeding.
- Body Mass Index (BMI): Typically 40 or higher, classifying as morbidly obese, or BMI of 35-40 with serious obesity-related health conditions
- Documented history of failed weight loss attempts through conventional methods
- Age requirements: Generally between 18-65 years, though exceptions exist based on individual health assessment
- Psychological stability and understanding of lifelong lifestyle changes required
- Absence of alcohol or drug dependency issues that could compromise recovery
- Commitment to long-term follow-up care and lifestyle modifications
Patients considering gastric bypass for obesity must complete several mandatory preparatory steps before receiving approval for the procedure:
- Comprehensive medical evaluation including cardiac, pulmonary, and metabolic assessments to confirm suitability for anesthesia and surgery
- Nutritional counseling to understand postoperative dietary requirements and prepare for significant eating habit changes
- Psychological evaluation to assess readiness for lifestyle changes and identify potential emotional challenges
- Smoking cessation at least six weeks prior to surgery to reduce surgical complications
- Participation in educational sessions about morbid obesity surgery and its implications
Healthcare providers use these gastric bypass requirements to identify patients who will benefit most from the procedure while minimizing risks. The multidisciplinary approach ensures that candidates are physically and emotionally prepared for this significant medical intervention. Understanding the Gastric Bypass Complications Timeline is crucial to evaluating the long-term effectiveness of the gastric bypass surgery purpose. This knowledge helps healthcare providers tailor post-operative care to each patient’s individual needs.
Gastric Bypass Surgery Process and Digestive System Modifications
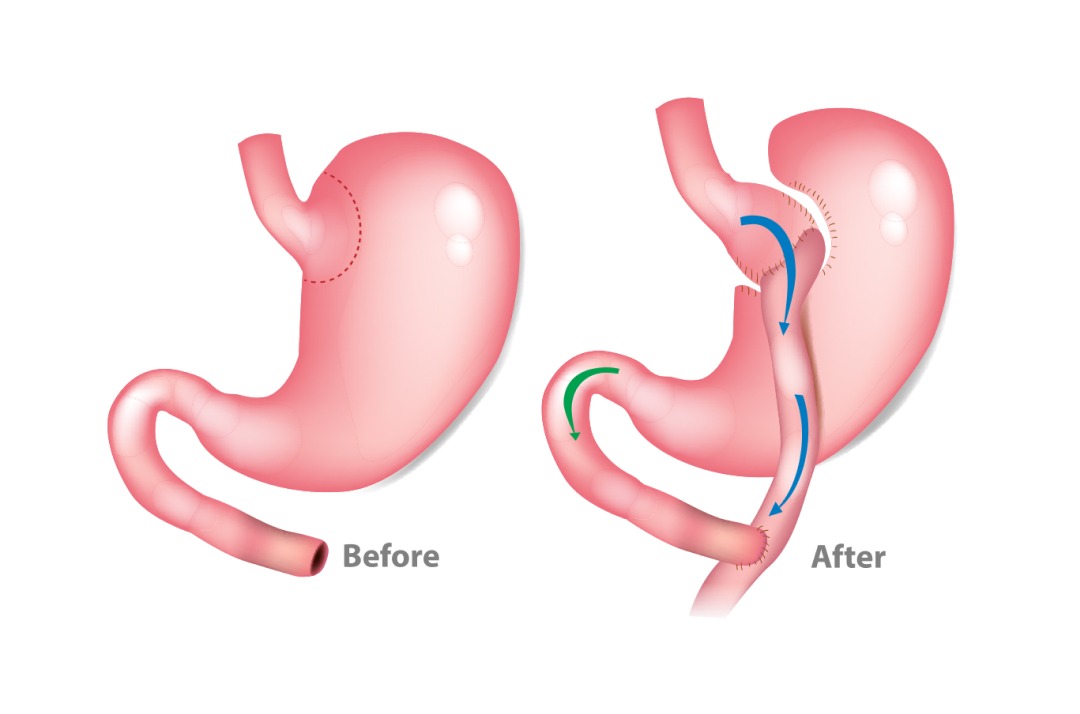
Gastric bypass surgery fundamentally alters the digestive system’s anatomy to facilitate weight loss. This permanent modification changes how food travels through the digestive tract and affects nutrient absorption.
Step-by-Step Gastric Bypass Surgery Procedure
- Anesthesia administration begins the gastric bypass operation, ensuring the patient remains unconscious throughout the procedure.
- Surgical access is established either through laparoscopic small incisions or traditional open surgery methods.
- Creation of a small stomach pouch by dividing the upper section of the stomach, reducing its capacity to approximately 30ml.
- Small intestine division occurs at a specific point, separating it into two segments.
- Roux limb creation by connecting the lower portion of the small intestine directly to the newly formed stomach pouch.
- Digestive loop reconnection joins the bypassed stomach section and upper intestine back to the lower portion of the small intestine.
- Surgical closure completes the procedure after confirming proper connections and absence of leaks.
Digestive System Modifications After Surgery
- Reduced stomach capacity as the functional stomach size decreases from approximately 1500ml to a 30ml pouch.
- Bypassed stomach section remains in place but no longer receives food directly, still producing digestive juices.
- Altered food pathway directs nutrients directly from the small pouch to the middle section of the small intestine.
- Digestive enzyme introduction delay occurs as pancreatic enzymes and bile meet food further down the digestive tract.
- Shortened digestive tract reduces the surface area for calorie and nutrient absorption.
- Hormonal changes affect hunger signals, satiety, and metabolic regulation throughout the body.
The stomach reduction surgery creates a dual mechanism for weight loss: restrictive effects from the smaller stomach pouch and malabsorptive effects from the bypassed portion of the small intestine. How gastric bypass works involves both limiting food intake and reducing the body’s ability to absorb calories and nutrients from consumed food.
Risks and Complications Assessment
Gastric bypass surgery risks and potential complications require thorough consideration before undergoing this bariatric procedure. Medical professionals categorize these risks as short-term (perioperative) and long-term complications.
- Immediate surgical risks: These include bleeding (occurring in 1-4% of patients), infection at incision sites, blood clots (deep vein thrombosis), and anesthesia-related complications. Research indicates respiratory problems may develop in approximately 5% of cases.
- Gastrointestinal complications: Gastric bypass surgery side effects often include dumping syndrome (affecting up to 85% of patients), where food moves too quickly from the stomach to the small intestine, causing nausea, vomiting, and diarrhea.
- Nutritional deficiencies: The altered digestive tract creates malabsorption of essential nutrients including iron, calcium, vitamin B12, and vitamin D. Studies show nearly 50% of patients develop deficiencies without proper supplementation.
- Bowel obstruction: This potentially life-threatening condition occurs in 2-4% of patients due to internal hernias or adhesions from surgical scarring.
- Anastomotic leaks: This serious complication involves leakage at surgical connection points, occurring in 1-5% of procedures and requiring immediate medical attention.
- Marginal ulcers: These painful sores develop at the junction between the stomach pouch and small intestine in approximately 5-15% of patients.
- Gallstone formation: Weight loss acceleration increases gallstone risk, affecting nearly 30% of gastric bypass patients.
- Reversibility concerns: While technically possible, the question “is gastric bypass reversible” has complicated answers. Reversal procedures carry significant risks and anatomical changes may not fully restore original function. Complete reversal becomes increasingly difficult as time passes after the initial surgery.
Recovery and Post-Surgery Effects
Gastric bypass recovery involves significant physiological adaptations as your body responds to both surgical changes and reduced food intake. Understanding what happens to your body after gastric bypass surgery helps manage expectations during the healing journey.
- Initial recovery phase requires careful monitoring of vital signs and surgical wounds
- Rapid weight loss occurs in the first 3-6 months, often 30-40% of excess weight
- Nutritional adjustments become necessary as your body adapts to the new digestive pathway
- Hormonal changes affect hunger signals, with decreased ghrelin production reducing appetite
- Metabolic improvements often appear before significant weight loss becomes visible
- Skin elasticity challenges may emerge as weight decreases rapidly
Your gastric bypass surgery recovery time follows a predictable timeline, though individual experiences vary based on pre-surgical health and adherence to post-operative guidelines:
- Hospital stay (2-3 days): Medical staff monitors for immediate complications while managing pain
- Liquid diet phase (2-4 weeks): Allows surgical connections to heal properly while providing essential nutrition
- Soft food transition (4-6 weeks): Gradual introduction of pureed and soft foods as tolerance builds
- Regular activity resumption (6-8 weeks): Most patients return to normal activities with continued dietary restrictions
- Stabilization period (6-12 months): Weight loss becomes more predictable as the body adapts to changes
Before and after gastric bypass surgery photos often showcase dramatic transformations, but these visual changes represent only part of the comprehensive health improvements. Most patients experience significant metabolic benefits including improved blood pressure, reduced joint pain, and enhanced mobility during recovery.
Surgery Outcomes and Success Rates
| Measurement | Short-term Results (1-2 years) | Long-term Results (5+ years) |
|---|---|---|
| Excess Weight Loss | 60-80% | 50-70% |
| Type 2 Diabetes Remission | 80-90% | 60-70% |
| Hypertension Improvement | 70% | 60% |
| Sleep Apnea Resolution | 85% | 75% |
The table above illustrates the remarkable effectiveness of gastric bypass surgery for weight loss across different timeframes. These statistics demonstrate why Roux-en-Y gastric bypass procedure remains one of the most performed bariatric surgeries worldwide.
- Significant weight reduction: Studies show patients typically lose 60-80% of excess weight within the first two years
- Sustainable results: 50-70% of excess weight loss maintained after 5+ years, though some weight regain may occur
- Health improvements: Substantial reduction in obesity-related comorbidities, particularly diabetes and cardiovascular conditions
The gastric bypass surgery success rate varies between individuals, with UK patients experiencing similar outcomes to global averages. Research confirms that most patients maintain substantial weight loss long-term, making weight control surgery a reasonable option for those who meet clinical guidelines when conventional methods fail.