The pursuit of effective obesity treatments has long driven medical innovation, with surgical interventions representing a significant frontier. Among these, the Roux-en-Y gastric bypass (RYGB) stands as a cornerstone procedure, demonstrating consistent and substantial weight loss outcomes. Its enduring relevance is underscored by extensive clinical data, validating its efficacy and safety profile over decades of practice. This intricate surgical technique, first described in 1967, has evolved into a sophisticated methodology, consistently contributing to improved metabolic health for countless individuals. The meticulous anatomical rearrangements involved in RYGB distinguish it from other bariatric approaches, leading to unique physiological adaptations. Understanding these fundamental principles is crucial for comprehending its profound impact on patient well-being and long-term health trajectories.
Table of Contents
Comparing Different Types of Weight Loss Surgeries
Weight loss surgery encompasses several distinct procedures, each designed to address obesity through different mechanisms. The roux-en-y gastric bypass surgery stands among the most established bariatric procedures, alongside sleeve gastrectomy, gastric banding, and duodenal switch operations. Understanding what is the difference between gastric bypass and roux-en-y becomes clearer when recognizing that Roux-en-Y represents the most common gastric bypass technique performed globally.
The comparison below illustrates key differences between major weight loss surgery options, highlighting why the RYGB procedure maintains its position as a gold standard in bariatric medicine.
| Surgery Type | Weight Loss Expectation | Recovery Time | Mechanism | Long-term Success |
|---|---|---|---|---|
| Roux-en-Y Gastric Bypass | 60-80% excess weight | 4-6 weeks | Restriction + Malabsorption | 85% maintain loss at 5 years |
| Sleeve Gastrectomy | 50-70% excess weight | 2-4 weeks | Restriction only | 70% maintain loss at 5 years |
| Gastric Banding | 40-60% excess weight | 1-2 weeks | Restriction only | 45% maintain loss at 5 years |
| Duodenal Switch | 70-85% excess weight | 6-8 weeks | Restriction + High Malabsorption | 80% maintain loss at 5 years |
Weight loss surgery roux-en-y demonstrates superior outcomes through its dual-action approach. The procedure creates both physical restriction through stomach size reduction and metabolic changes through intestinal rerouting. This combination addresses hormonal factors influencing hunger and satiety more effectively than purely restrictive procedures.
Clinical data reveals that patients undergoing the roux-en-y gastric bypass surgery experience significant improvementin obesity-related conditions. Diabetes remission rates reach 83% within the first year, while hypertension improvement occurs in 68% of patients. These outcomes exceed those typically achieved through sleeve gastrectomy or gastric banding alone.
The RYGB procedure requires greater surgical expertise and carries slightly higher initial risks compared to sleeve gastrectomy. However, its proven track record spanning over 30 years of refinement makes it the preferred choice for patients with severe obesity, particularly those presenting with metabolic syndrome or type 2 diabetes complications. While both RYGB and sleeve gastrectomy have their merits, the Lap Band Surgery Guide provides insights into alternate procedures that some patients might consider. Ultimately, choosing the right surgical approach depends on individual health needs and a thorough consultation with a healthcare professional.
How Does Roux-en-Y Surgery Change Your Anatomy to Help You Lose Weight?
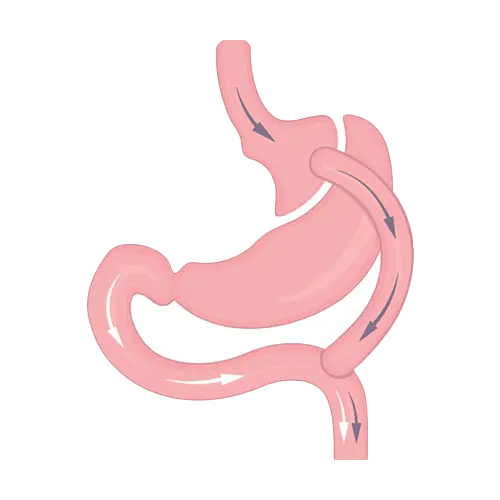
Roux-en-Y gastric bypass fundamentally restructures your digestive anatomy through precise surgical modifications that create powerful weight loss mechanisms. This roux-en-y reconstruction transforms your stomach and small intestine configuration to establish both restrictive and malabsorptive effects.
The anatomical changes from lap roux en y surgery create a sophisticated new digestive pathway:
- Small stomach pouch creation: The surgeon divides your stomach, forming a 15-30ml pouch from the upper portion while the remaining stomach becomes inactive. This roux-en-y stomach pouch dramatically limits food intake capacity, generating early satiety signals after consuming minimal quantities.
- Gastrojejunostomy connection: The roux-en-y gastrojejunostomy links your new stomach pouch directly to the jejunum, bypassing the duodenum completely. This connection measures approximately 12mm in diameter, preventing rapid food passage while maintaining adequate drainage.
- Roux limb construction: The alimentary limb carries food from your stomach pouch to the Y-connection point, typically measuring 75-150cm in length. This roux limb eliminates acid and enzyme exposure from pancreatic and biliary secretions during initial digestion phases.
- Biliopancreatic limb formation: This segment transports bile and pancreatic enzymes from your bypassed stomach and duodenum to the Y-junction. The biliopancreatic limb ensures essential digestive enzymes reach the common channel for nutrient processing.
- Common channel establishment: The Y-limb represents where the roux limb and y-limb merge, creating the 150-200cm common channel where nutrient absorption occurs. This shortened absorption zone reduces caloric and nutrient uptake significantly.
Understanding roux-en-y anatomy reveals how these modifications generate 60-70% excess weight loss within two years. The roux-en-y meaning encompasses both mechanical restriction and metabolic changes that alter hunger hormones like ghrelin and GLP-1.
This roux-en-y patient information demonstrates how the procedure creates multiple weight loss mechanisms simultaneously. The small stomach pouch restricts portion sizes, while the bypassed intestinal segments reduce nutrient absorption capacity. Additionally, the altered gut hormone production decreases appetite and increases satiety responses.
The sophisticated roux-en-y surgery design ensures food travels through distinct pathways before mixing with digestive enzymes, maximizing both restrictive and malabsorptive benefits for sustainable weight management.
Step-by-Step Guide to Laparoscopic Roux-en-Y Procedure
The laparoscopic roux-en-y gastric bypass surgery follows a precise sequence of surgical steps that our surgical team has refined through extensive experience with bariatric procedures. This minimally invasive approach ensures optimal patient outcomes whilst maintaining the highest safety standards.
- Patient positioning and trocar placement – The patient is positioned supine with legs apart. Five to six small incisions (5-12mm) are created for trocar insertion. The surgeon establishes pneumoperitoneum with CO2 insufflation at 15mmHg pressure. This laparoscopic approach provides superior visualisation compared to open techniques.
- Creation of the gastric pouch – Using an endoscopic linear stapler, the surgeon divides the stomach horizontally approximately 2cm below the gastroesophageal junction. The laparoscopic roux-en-y procedure requires creation of a 15-30ml gastric pouch. Additional staple lines complete the vertical division, creating the small upper stomach pouch.
- Gastrojejunostomy construction – The jejunum is identified approximately 50cm from the ligament of Treitz. An antecolic, antegastric approach is typically employed. The surgeon creates a 12-15mm gastrojejunal anastomosis using either circular or linear staplers, followed by hand-sewn reinforcement of the anastomotic line.
- Jejunojejunostomy formation – The laparoscopic roux-en-y gastric bypass steps include measuring a 75-150cm Roux limb from the gastrojejunostomy. The jejunojejunostomy is constructed using stapling techniques, creating the side-to-side anastomosis. The surgeon closes the mesenteric defects to prevent internal herniation.
- Gastric bypass stapling verification – Each staple line undergoes meticulous inspection for haemostasis and integrity. Methylene blue testing through an orogastric tube confirms anastomotic integrity. The laparoscopic roux-en-y bypass technique allows for enhanced visualisation of all staple lines under magnification.
- Leak testing and closure – Air insufflation testing ensures no anastomotic leaks exist. The surgeon irrigates the abdomen and achieves complete haemostasis. Trocars are removed under direct vision, and fascial defects ≥10mm receive closure. Skin incisions are closed with absorbable sutures or skin adhesive.
Our surgical experience demonstrates that the laparoscopic roux-en-y gastric bypass surgery typically requires 90-180 minutes depending on patient anatomy and surgeon expertise. The procedure’s success depends on precise stapling techniques, meticulous attention to anastomotic construction, and thorough leak testing protocols. Each step builds upon the previous one, creating the definitive anatomical reconstruction that characterises this gold-standard bariatric procedure.
Benefits and Risks: Making an Informed Decision
Understanding the comprehensive pros and cons of roux-en-y gastric bypass requires careful evaluation of both immediate and long-term outcomes. This transformative procedure delivers significant health improvements while carrying inherent surgical risks that demand thorough consideration.
Major advantages include substantial weight reduction, with patients typically losing 60-80% of excess weight within the first two years. The procedure effectively resolves type 2 diabetes in approximately 75% of cases, while dramatically improving hypertension, sleep apnea, and cardiovascular health markers.
Primary roux-en-y complications encompass both surgical and nutritional challenges:
- Dumping syndrome affecting 20-30% of patients
- Nutritional deficiencies requiring lifelong supplementation
- Anastomotic leaks occurring in 1-2% of cases
- Bowel obstruction risks
- Marginal ulceration
- Gallstone formation
Long-term roux-en-y bypass risks and benefits demonstrate sustained effectiveness alongside manageable complications. Most patients maintain significant weight loss while experiencing improved quality of life and reduced obesity-related mortality.
The following data illustrates outcomes spanning two decades post-surgery:
| Timeframe | Weight Maintenance | Complication Rate | Patient Satisfaction |
|---|---|---|---|
| 5 Years | 65-75% excess loss | 15-20% | 85-90% |
| 10 Years | 55-65% excess loss | 25-30% | 80-85% |
| 20 Years | 50-60% excess loss | 35-40% | 75-80% |
Twenty years after roux-en-y gastric bypass, research demonstrates sustained benefits despite gradual weight regain in some patients. Long-term studies reveal maintained diabetes remission in 60-70% of cases, with significant cardiovascular protection persisting throughout the follow-up period.
Nutritional monitoring becomes increasingly critical over time, with vitamin B12, iron, calcium, and folate deficiencies requiring vigilant management. Bone density concerns emerge, particularly affecting post-menopausal women.
The decision ultimately depends on individual risk tolerance, commitment to lifestyle modifications, and severity of obesity-related health conditions. Patients achieving optimal outcomes demonstrate consistent adherence to dietary guidelines, supplement regimens, and regular medical follow-up. Successfully navigating the roux-en-y journey requires understanding that while complications exist, the procedure’s proven track record of transforming lives through sustained weight loss and health improvements makes it a powerful tool against severe obesity.